Positive Health Online
Your Country

Stress as Cause of Heart Attacks - The Myogenic Theory
by Carlos ETB Monteiro(more info)
listed in heart, originally published in issue 222 - May 2015
The Myogenic Theory
The theory that heart attacks begin in the heart itself - the Myogenic Theory - and not in the arteries, was developed by my father-in-law, the Brazilian cardiologist, Quintiliano H de Mesquita, who died in 2000.[1] In this article, I propose to describe the history of the myogenic theory for a public that is largely unaware of this alternative theory since its introduction in 1972.[2,3]

Dr Quintiliano H. de Mesquita flanked by his daughter Solange and Carlos Monteiro (1982)
In addition to the myogenic theory, Dr Mesquita developed the concept of ventricular aneurysm surgery. Ventricular aneurysm is a complication that can occur after a heart attack, arising from a patch of weakened tissue in a ventricular wall. The surgery was first performed by Dr Charles Bailey in 1954, and is still often performed on patients after a heart attack. My father-in-law also made the first diagnosis of right ventricular infarction by the electrocardiogram in 1958. He was the author of more than thirty pioneer contributions to medical literature in the field of cardiology.
The main reasons that led Dr Mesquita to break with the conventional thrombosis theory of heart disease - which states that the heart attack is caused by blocked arteries - are as follows:
- Clinical observations showing the absolute lack of efficacy of anticoagulants in the treatment of unstable angina pectoris. Unstable angina is considered to be a stage leading to myocardial infarction;
- The strong correlation of myocardial infarction with stress or unusual physical activity;
- Frequent coronary angiographies showing no obstructions in the presence of myocardial infarction;
Dr Mesquita’s suspicion about the coronary thrombosis theory increased when he found that:
- Many anatomic-pathological studies have demonstrated no relationship between thrombus and infarction, which led many authors since the 1940s to consider coronary thrombosis - the clot in the arteries - as a consequence of acute myocardial infarction, not its cause;
- The development of coronary thrombus after a heart attack, demonstrated experimentally.
Along with these observations, Dr Mesquita also found that since the beginning of the twentieth century, several doctors had used cardiotonics (cardiac glycosides like digoxin, digitoxin, and ouabain / strophanthin), with remarkable results in the treatment of both stable angina pectoris and acute myocardial infarction. Among these were the American Dr James Bryan Herrick (in 1912), even though he was an important supporter of the coronary thrombosis (thrombogenic) theory as the cause of heart attacks. Another was Dr Ernst Edens (1934) from Germany.
In 1975, Dr Mesquita was awarded the Ernst Edens Traditionspreis by the International Society to Fight Infarction (Internationale Gesellschaft für Infarktbekämpfung), located near Stuttgart, Germany. Its president at the time was Dr Berthold Kern, who has used sublingual strophanthin in more than fifteen thousand patients with angina or myocardial infarction.
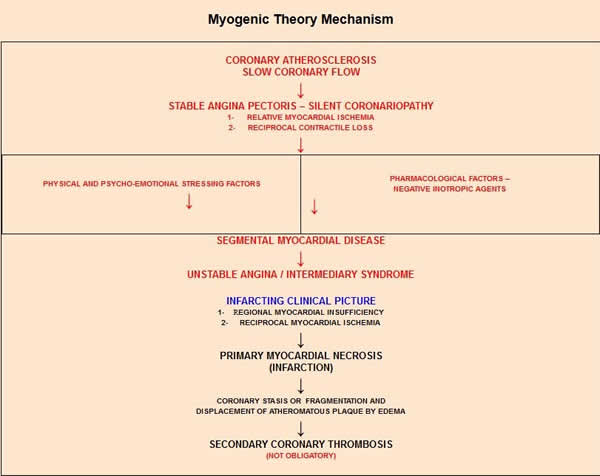
Development of Myogenic Theory
Assuming that unstable angina pectoris (chest pain) could be the result of a regional myocardial failure (and not a clogged artery), with episodic, but reversible, manifestations, Dr Mesquita came to the conclusion that only the therapeutic correction by a cardiotonic would be able to reverse the clinical picture and prevent the myocardial infarction. Eventually he came to see heart disease as a three-stage process:
Stage I: Stable angina (chest pain), an intermittent and reversible process indicating regional myocardial ischemia (restriction in blood supply to the tissues) caused by physical exertion or psycho-emotional stress, and loss of regional myocardial contractility;
Stage II: Unstable angina (more severe chest pain), a process that is still reversible, indicating regional myocardial insufficiency, which is episodic, spontaneous, and reversible, with regional myocardial ischemia (restriction in blood supply);
Stage III: Acute myocardial infarction (heart attack), an irreversible process characterized by regional myocardial insufficiency restrained and reversible only by cardiotonics; absolute regional myocardial ischemia; circulatory stagnation followed by myocardial necrosis (death to the heart tissue); satellite coronary artery stasis, with possible fragmentation or displacement of atheromatous plaque due to the heart attack and vascular processes; and, on occasion, secondary coronary thrombosis (blockage of a coronary artery).
After he formulated the myogenic theory in early 1972, Dr Mesquita sought to start clinical investigations by testing cardiotonics in unstable angina. During his previous thirty-one years of medical practice, he found that all treatments for unstable angina were failures. His many years of clinical experience led him to conclude that intravenous strophanthin (K or G) was the most reliable cardiotonic in all cases of acute myocardial infarction complicated by heart failure.
Two days after coming up with his theory, Dr Mesquita received in his medical office an engineer of fifty-seven years who had been affected for the previous fifteen days by daily outbreaks of acute coronary insufficiency, unresponsive to treatment, even to rapid-acting nitrates. According to Dr Mesquita, this individual was predestined to provide the therapeutic proof of his new theory. The patient had come to his medical office because he was on the verge of a heart attack and his personal physician passively awaited the event which, he said, could be lethal.
Dr Mesquita gave him an injection of strophanthin-K (1/4 Kombetin mg) plus dipyridamole (Persantine 20mg), plus an oral coronary vasodilator drug, prenylamine (Synadrin 180mg/ day), for ten days, along with bed rest in his home. When he returned to Dr Mesquita’s office, the patient was declared cured because the symptoms had ceased after the first injection.
The treatment, confirmed by angiogram and ventriculogram, was so successful that Dr Mesquita felt confident of his theory. At this point, he coined his new concept the myogenic theory of myocardial infarction.
Cover in Portuguese of the book Myogenic Theory of Myocardial Infarction
Summary Translation of the book to English
What About Atherosclerosis?
If the heart attack begins in the heart muscle itself, what is the role of atherosclerosis -hardening of the arteries - in heart disease? In his book, Myogenic Theory of Myocardial Infarction (1979),[4] Dr Mesquita explained that the triggering cause represented by physical exertion or psycho-emotional stress increases the activity of the heart in the face of the fixed or deficient flow in the coronary blood supply, producing the regional ischemia. This lack of blood supply then leads to the loss of contractility within a few seconds, along with reduced ejection phase, increased volume and final diastolic pressure during the ischemia, along with an overload in contractility of normal regions of the heart.
Each episode of myocardial ischemia by stress or emotion affects the cardiac muscle segment dependent on the affected coronary artery, compromising the myocardial structure. Over time the repeated ischemic manifestations in the same regions of the heart will cause pathological structural changes, different from the unaffected surrounding non-ischemic areas of normal structure. In his book, Myogenic Theory of Myocardial Infarction,[4] Dr Mesquita says, “Thus, the coronary disease contributes to the deterioration of the ventricular segment, constituting areas of myocardial sclerosis or segmental myocardial disease, the possible future site of the myocardial infarction.”
Stress and the Heart
One point that needs emphasis is the fact that most risk factors for coronary heart disease, including smoking, hypertension and diabetes, are associated with autonomic nervous system dysfunction with overactive sympathetic system (fight or flight response), leading to elevation of stress hormones (adrenaline and noradrenaline).
Acute stress or chronic stress overload often represents the final blow to a vulnerable segment of the heart muscle, affected by chronic coronary disease, triggering the acute myocardial infarction. However, the impact of acute stress may also trigger an MI in patients with normal coronary arteries. Several studies have shown a close connection between catecholamine (adrenaline and noradrenaline stress hormones) and myocardial infarction. The hyperactivity of the sympathetic nervous system, with an intense outflow of catecholamine, also occurs in unstable angina, although to a lesser extent and for a shorter period of time than in acute myocardial infarction.
Takotsubo cardiomyopathy, also known as ‘broken heart syndrome’, is a sudden temporary weakening of the heart muscle, one obviously triggered by acute stress. In broken heart syndrome the patient has an intense outflow of catecholamine, even greater than in patients with acute myocardial infarction. Takotsubo cardiomyopathy simulates an evolving myocardial infarction clinical picture. It occurs in patients with no signs of coronary heart disease. This is obviously a condition where the aetiology is better explained by the myogenic theory of heart disease.
In addition to intense physical activity, particularly in sports competition, or unusual physical efforts that surpass the limits of the individual’s heart condition, or the heavy use of stimulant drugs, there are many risk factors for acute myocardial syndromes based on recent severe stress situations or sudden emotional upset. These include marital separation or divorce, retirement or loss of work, loss of revenue or business failure, family conflicts, serious personal injury or illness, death or illness of a close family member, shock of a surprise party, armed robbery or other kinds of violence, heated discussion, threats or acts of war - even earthquakes and other frightening natural disasters.
The most common immediate cause of sudden cardiac death is ventricular fibrillation. Ventricular fibrillation is a condition in which there is uncoordinated contraction of the cardiac muscle of the ventricles in the heart, making them quiver rather than contract properly. Ventricular fibrillation may be triggered by autonomic nervous system disturbance due to acute stress.
Cardiotonics
The heart is nourished by two main coronary arteries, the right and the left, with branches to supply oxygen and blood throughout the heart muscle, and also by a network of collateral blood vessels. According to Dr Mesquita, an important role of the cardiotonic remedy is to enhance the effects of collateral coronary circulation and ensure the preservation of the ischemic myocardium (the heart tissue where blood flow is blocked or reduced). As noted in his book: “The collateral coronary circulation network is not always able to prevent myocardial infarction, because it develops depending on the anatomical features of the obstructive process, and also it is not always sufficient to face the demands of the coronary patient’s physical activity.”
Indeed, collateral coronary circulation bypasses the blockages in the coronary arteries, supplying enough oxygenated blood to enable the cardiac tissue to survive and recover. A recent meta-analysis confirmed the observation that heart disease patients with a well-developed collateral coronary circulation have an improved survival compared with patients with less developed collaterals.[5]
Cardiotonics also act to harmonize the differences in contractility between both the ischemic and non-ischemic regions of the heart and allow for coordinated function among the segments.
Findings showing that cardiotonics such as ouabain/strophanthin and digitalis (digoxin and digitoxin) have a direct relationship between dosage and myocardial contractile force were discussed by Charles C. Wycoff in 1969. Based on these findings, he raised the hypothesis of a possible beneficial effect from digitalis in a dose much lower than that which was considered effective in the past. Noting that in many clinical settings, digitalis showed beneficial effects during surgery and for chronic hypertension, angina, acute myocardial infarction, and healed myocardial infarctions, Wycoff argued for a much wider use of digitalis than the generally accepted indications for this drug.[6]
Cardiotonics may offer other possible benefits for ischemic heart disease, independent of their effects on the strengthening of heart muscle contraction, through stress reduction by the improvement of baroreceptor function (sensors in the blood vessels that help to maintain blood pressure at nearly constant levels), reduction of sympathetic nervous system activity, support of the vagus nervous system, and reduction in secretion of catecholamines.[7,8,9]
Cardiotonic drugs have been used for over two hundred years to treat patients with heart failure where there is reduced force of muscle contraction, due to overloading of the ventricle. As predicted by Wycoff, recent studies have indicated that a beneficial effect on morbidity and mortality from digoxin, the most popular cardiotonic drug for heart failure, is seen at lower rather than higher doses.[10-12] By the way, it has been known for more than one hundred years that heart failure is characterized by excessive sympathetic nervous system activity.
Lactate In The Heart
The heart is an organ of high metabolic activity - it cannot rest as can other body muscles. Chronic or acute elevated catecholamine release may accelerate myocardial glycolysis leading to a significant increase in lactate production. Lactic acidosis results from increased production of lactate, the final product in the pathway of glucose metabolism. Studies show that lactate accumulation predicts ischemic myocardial necrosis.[13]
Measurement of arterial blood lactate is considered a consistently useful prognostic indicator of survival or fatality in patients with acute myocardial infarction.[14] A recent study has shown a significant association of elevated plasma lactate levels with heart failure and all-cause mortality.[15] Therefore the reduction of stress due to cardiotonic use may indirectly lower lactate production by the heart muscle. Bruno Levy and colleagues postulate that adrenaline increases lactate formation by an increase in the NA+K+ - ATPase activity,[16] which can be inhibited through cardiotonics that are sodium pump inhibitors. The link between adrenaline and increased NA+K+ - ATPase activity is well established.
Robert Tennant and Carl J Wiggers hypothesized in 1935 that the accumulation of lactic acid and decrease in pH were linked to myocardial contractile failure after the occlusion of the coronary arteries.[17] Tennant also proposed in 1935 that tissue acidosis might account for contractile failure during myocardial ischemia.[18]
The influence of adrenaline on lactic acid production was first noticed by Carl F Cori in 1925.[19] In 1964, John R. Williamson confirmed the effects of adrenaline infusion on the increased production of lactate in isolated heart tissue, up to five times the normal production.[20] (Note: Lactate and lactic acid are not synonymous. Lactic acid is a strong acid which, at physiological pH, is almost completely ionized to lactate.)
Dr Mesquita reveals in his writings a different source generating excess lactate in the heart muscle leading to the infarction: “The failure of the myocardial ischemic area, losing regional contractility and relaxing the myocardial fibre, would become stagnant and without contractility, thus developing anaerobic metabolism - with the deposit of lactate and catabolites plus depletion of energetic phosphate.”[4] According to Dr Mesquita, the anaerobic metabolism represents a step toward the myocardial infarction and necrosis in the particular region of the heart.
A seminal paper published in the November 2013 The Lancet Diabetes & Endocrinology reviewed recent findings showing that hyperlactatemia is not a consequence of anaerobic metabolism, tissue hypo-perfusion or reduced oxygen to the cells. The authors say in their conclusion that “In all studied settings, lactate production happens under fully aerobic conditions. Such hyperlactatemia is probably indicative of a stress response, with increased metabolic rate and sympathetic nervous system activation inducing a state of accelerated glycolysis and modified bioenergetic supply.”[21]
Increased blood lactate levels are also associated with cigarette smoking,[22]diabetes,[23,24] hypertension[25] and atherosclerosis,[26]proven risk factors for heart disease.
Endogenous Cardiotonics
The recent discovery of endogenous (made in the body) cardiotonic steroids (also known as digitalis-like compounds and endogenous cardiac glycosides - digoxin, digitoxin, ouabain/ strophanthin, proscillaridine, etc.) - isolated from human tissues and body fluids, may represent a strong new argument for the myogenic theory of myocardial infarction. Elevated concentrations of endogenous cardiotonics have been found under different clinical conditions such as sodium imbalance, hypertension, cardiac arrhythmias, chronic renal failure, congestive heart failure, and acute myocardial infarction. Vigorous physical exercise as well as physiological stress situations may also elevate the concentration of endogenous cardiotonics in the human body. We can surmise that the cardiotonics found in nature, like digoxin and ouabain/strophanthin, may compensate for a deficient production of endogenous cardiotonic steroids by the human body and thus support cardiac metabolism and protect the heart from the infarction, as proposed in the myogenic theory.
Recent Studies
Sudden emotional stress[35] or strenuous exercise[36] may precipitate temporary and reversible regional myocardial failure in patients without cardiovascular disease. Moreover, a study published in April 2014 demonstrated that in a large multi-ethnic cohort without symptoms of cardiovascular disease at enrolment, elevated resting heart rate (which is related to sympathetic dominance over the parasympathetic system) was strongly associated with the development of regional and global left ventricular dysfunction, as well as the incidence of heart failure.[37]
In 2006 the same group provided evidence of a direct relationship between subclinical atherosclerosis and reduced regional myocardial function in asymptomatic individuals - with alterations in myocardial contractility - without previous clinical cardiovascular disease.[38] Left ventricular dysfunction classification also includes regional myocardial failure (or insufficiency), a term coined by Tennant and Wiggers in 1935,[17] which was adopted by Mesquita in 1972, but later designated by others as “myocardial stunning.” These striking findings provide cutting edge evidence to the pathophysiological mechanism of the myogenic theory of myocardial infarction.

(L-R) David Diamond, Malcolm Kendrick, Carlos Monteiro, and Paul Rosch
during a break in proceedings at the conference.
In November of 2012, the author made a tribute to Dr Mesquita during the Fourth International Conference of Advanced Cardiac Sciences - the “King of Organs” conference, held in Saudi Arabia. He has presented some of Dr Mesquita’s pioneering contributions to medical science, particularly regarding the pathophysiological and therapeutic concepts of the myogenic theory. The presentation covered the following topics: Coronary Thrombosis: Cause or Consequence of Myocardial Infarction?; Introduction and Fundamentals; Mechanism and Sequence of Events; Stress and Acute Myocardial Syndromes; and Benefits of Cardiotonic Drugs in Patients with Stable Ischemic Heart Disease, Unstable Angina, and Acute Myocardial Infarction.[5] The author is indebted to Dr Paul J Rosch, president of the American Institute of Stress, professor of medicine and psychiatry at New York Medical College, and member from the scientific committee, who suggested him as a speaker for this conference.[27]

Cover Image from ppt Myogenic Theory of Myocardial Infarction
Pathologic Q Waves
Pathologic Q waves, as seen on an electrocardiogram, are usually a sign that indicates current or prior myocardial infarction. They show the absence of electrical activity. A myocardial infarction can be thought of as an electrical ‘hole’, since scar tissue is electrically dead and therefore results in electrocardiographic Q waves. Pathologic Q waves are not an early sign of acute myocardial infarction, but generally take several hours to days to develop. Once pathologic Q waves have developed they rarely go away. The use of pathologic Q waves in electrocardiographic diagnosis of acute myocardial infarction has decreased in clinical practice during the last decades. In 2000, medical boards proposed the first official redefinition of myocardial infarction, followed by others, which were published in 2007 and 2012, with the endorsement of the European Society of Cardiology, the American College of Cardiology Foundation, the American Heart Association, and the World Heart Federation.
These redefinitions of myocardial infarction implied that any signs of necrosis in the setting of myocardial ischemia, regardless of the pathobiology, should be labelled as MI. This favoured using the protein troponin as the preferred biomarker for MI. (Troponin is considered a highly specific marker for myocardial infarction or heart muscle cell death.)
These redefinitions also spread the use of ST segment elevation in electrocardiographic diagnosis of MI. However, troponin levels may be elevated in other cardiac and non-cardiac disorders, not just in myocardial infarction. Also, both ST segment elevation and ST segment depression may be associated with other ischemic settings, with no infarction. This strategy resulted in more cases being diagnosed, adding patients with conditions not so severe and consequently leading to the decrease in statistical indices of global mortality for myocardial infarction. Despite the significant drop in mortality using this new broadened definition for myocardial infarction, recent studies claim that “Q-waves are a major determinant of in-hospital mortality, and targeted interventions should be directed to these high-risk patients.”[32] Incidentally, studies have shown that mental stress[33] and exercise[34] may induce cardiac troponin elevation, unrelated to myocardial injury, leading many people to unnecessary hospital admissions and invasive procedures.
Thrombogenic Theory Versus Myogenic Theory of Heart Disease
Let’s look at the different philosophies, therapeutics, and outcomes for the three stages of ischemic heart disease.
Stage One
The first stage is represented by symptomatic and myocardial stability, stable angina pectoris, and silent coronary cardiomyopathy (disease of the heart muscle), with and without previous infarction. In this stage, the main therapeutic focus of the thrombogenic theory is to maintain the coronary blood flow by correcting or circumventing the obstructions in the coronary arteries caused by atherosclerosis and to avoid coronary thrombosis thought to lead to myocardial infarction. This is accomplished through procedures like angioplasty, stents, and coronary atherectomy; the creation of grafts in the coronary artery; bypass surgery; and by the use of drugs like coronary dilators, adrenergic beta-blockers, cholesterol-lowering agents like statins, anticoagulants and antiplatelet agents. The intention is to ensure the myocardial perfusion by improving the coronary blood flow; however, this strategy leaves the ventricular function to its own fate.
By contrast, the goals of the myogenic theory in the first stage of heart disease are to neutralize the reduced contractility effects of ischemia (restriction of blood supply to the tissues); to preserve the function of the ventricles (chambers of the heart); to prevent unstable angina, myocardial infarction, heart failure, and sudden death due to severe arrhythmias; to ensure permanent myocardial stability; to provide a peaceful, comfortable, and predominantly asymptomatic long survival; and to support the natural effects of coronary collateral circulation, when it is already established. These goals are accomplished by the prophylactic oral use of cardiotonics like low dose digoxin plus coronary dilators and ACE inhibitors (the last one indicated by Dr Mesquita since the 1990s).
An interesting study involved two groups of stable patients using the therapeutics recommended by the myogenic theory in the first stage of ischemic heart disease; these cases were followed by Dr Mesquita and colleagues.[28,29] The first group included 994 patients without prior infarction given cardiotonics, presenting over twenty-eight years the following morbidity and mortality:
- Myocardial infarction: 14 cases (1.4%);
- Heart failure mortality: 32 cases (3.2%);
- Sudden death: 72 cases (7.2%);
- Stroke mortality: 13 cases (1.3%);
- Cancer mortality: 14 cases (1.4%);
- Other causes of mortality: 11 cases (1.1%);
- Total mortality: 142 cases (14.2%) - (0.5% per year!);
- Mean age at death: 76 years.
The second group included 156 patients with prior infarction, also using cardiotonics, presenting over twenty-eight years the following morbidity and mortality:
- Recurrent MI: 8 cases (5.1%);
- Heart failure mortality: 17 cases (10.8%);
- Sudden death: 32 cases (20.5%);
- Stroke mortality: 7 cases (4.4%);
- Cancer mortality: 3 cases (1.9%);
- Other causes of mortality: 5 cases (3.2%);
- Total mortality: 64 cases (40.8%) - (1.45% per year!);
- Mean age at death: 72 years.
As a point of interest, we can compare total, cancer, and stroke mortalities, using the therapy recommended by the myogenic theory, with those found in The Heart Protection Study (HPS),[30] which had a follow-up of five years, involving 20,536 patients aged forty to eighty years with coronary heart disease, other vascular diseases, or diabetes. The HPS found a total mortality of 12.9 percent (2.58 percent per year). The specific mortality for cancer was 3.5 percent (0.70 percent per year) in patients taking statins and 3.4 percent (0.68 percent per year) in patients taking a placebo. Regarding the stroke mortality the HPS found a total of 0.9 percent (0.18 percent per year) in patients taking statins and 1.2 percent (0.24 percent per year) in patients taking placebo. Taking digoxin and other cardiotonics administered by Dr Mesquita and colleagues resulted in a much lower mortality rate for cancer (0.06 percent per year) and stroke (0.04 percent - 0.15 percent per year).
Stage Two
Stage two is represented by symptomatic and myocardial instability - unstable angina pectoris, either quiescent or pre-infarction. In this stage the primary focus of the thrombogenic theory of heart disease is to re-establish the coronary blood flow in the coronary arteries, partially or totally obstructed by atherosclerosis, with or without coronary thrombi, and to avoid the imminent myocardial infarction. The immediate therapeutic is the use of thrombolytics, coronary dilators, beta-blockers, anticoagulants, or antiplatelet drugs - plus coronary angioplasty, stents, coronary artery bypass surgery and coronary atherectomy.
The focus in the myogenic theory is the immediate correction of the regional and primary myocardial insufficiency responsible for the secondary myocardial ischemia, and restraining the quiescent angina pectoris episodes; reestablishment of the symptomatic and myocardial stability; and prevention of myocardial infarction. As with Stage One, the therapeutic action for the unstable angina is the use of cardiotonics plus a coronary dilator. In one hundred ninety-nine patients, Dr Mesquita found that this strategy led to an immediate interruption of the spontaneous episodes, with subsequent myocardial infarction reduced to 0.5 percent and a mortality rate of zero.[28]
Stage Three
The third stage is represented by acute myocardial infarction. The main focus in the thrombogenic theory is to re-establish the coronary flow interrupted by vasospasm or intracoronary thrombus. After the detection of complete obstruction of the coronary artery by cardiac catheterization, nitro-glycerine is used to control the vasospasms. If the obstruction persists, the patient is submitted to thrombolytic action followed by anticoagulant and antiplatelet agents. The symptomatic treatment is initiated with coronary dilators, beta blockers, and antiplatelets. In cases of partial coronary obstruction, patients undergo bypass surgery, stents, atherectomy or angioplasty. In cases of patients with coronary arteries angiographically normal, the explanation in general is the occurrence of spontaneous fibrinolysis (a process that prevents blood clots from growing and becoming problematic).
The three most common types of electrocardiographic diagnosis for the myocardial infarction are ST-segment elevation myocardial infarction, non-ST-myocardial infarction, and pathological Q waves.
In the Grace multinational observational study, which involved 21,688 cases with acute myocardial syndrome (STsegment elevation MI, non-ST-MI, or unstable angina), 9.1 percent died or experienced a non-fatal myocardial infarction between the hospitalization and the six-month follow-up.[31] Many studies have shown a thirty-day mortality for patients with Q-wave MI between 17 and 30 percent (Hutter et al, 1981; Scheinman and Abbott, 1973; Szklo et al, 1978; Cannon et al, 1976; Mahoney et al, 1980; Rigo et al, 1975; Connolly and Elveback,1985; etc.).
The first goal for Stage Three in the myogenic theory is to correct the regional myocardial insufficiency and reduce myocardial ischemia, halting the infarcting clinical picture immediately as the patient enters the coronary unit, seeking to avoid the infarction or to interrupt its evolution, or at least mitigate the attack. This includes reducing the size of infarction as well as preventing the secondary coronary thrombosis through the cessation of circulatory stagnation in the satellite artery of the infarction and in the compromised myocardial region. The immediate therapeutic is, again, a cardiotonic, given intravenously, plus coronary dilator.
As for the results of therapy with cardiotonics, without any invasive treatment, Dr Mesquita and his colleagues followed 1109 patients with a heart attack confirmed by Q waves. Mortality in the hospital was 12.2 percent; at thirty days from hospital release, it was an impressive 0.4 percent. Of patients under seventy years old, 9.7 percent died, while in patients over seventy years, 28.1 percent died.[28] Results are as follows:
- Ventricular extrasystoles: 24.1%;
- Partial AV block: 5.8%;
- Complete AV block: 4.6%;
- Atrial tachycardia: 1.7%;
- Flutter – atrial fibrillation: 4.4%;
- Tachycardia + ventricular fibrillation: 2.7%;
- Asystole: 4.5%;
- Cardiogenic shock: 2%;
- Acute pulmonary edema: 1.3%;
- Heart failure: 1%;
- Overall mortality in-hospital: 12.2%;
- Mortality in 30 days after the discharge from hospital: 0.4% (5 patients);
- Mortality by age: 9.7% in patients under 70 years and 28.1% in patients over 70 years.
References
1. Memorial to Dr Quintiliano H. de Mesquita at www.infarctcombat.org/qhm/homepage.html
2. What Causes Heart Attacks? by Dr Thomas Cowan. Published in Wise Traditions in Food, Farming and the Healing Arts, Fall 2007 at www.westonaprice.org/cardiovascular-disease/what-causes-heart-attacks
3. Two Heart Disease Theories, Same Therapeutic Treatment (cardiotonics), by Carlos Monteiro. Published in Dr Thomas Cowan’s Newsletter with an editorial entitled “Redefining Heart Disease” Dec 2005 at www.fourfoldhealing.com/2005/12
4. Quintiliano H. de Mesquita. Book Myogenic Theory of Myocardial Infarction, 1979. Summary in English at www.infarctcombat.org/LivroTM/parte8.htm
5. Pascal Meyer et al. The impact of the coronary collateral circulation on mortality: a meta-analysis. Eur Heart J 33 (5): 614-621. 2012.
6. Charles C. Wycoff. New Concepts of digitalis, Calif Med 1969, 111(6): 423 at www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1503737
7. Gheorghiade M, Adams KF, Colucci WS. Digoxin in the Management of Cardiovascular Disorders 109: 2959-2964. 2004.
8. Schobel HP et al. Contrasting effects of digitalis and dobutamine on baroreflex sympathetic control in normal humans, Circulation V84, 1118-1129. 1991.
9. Gutman Y, Boonyaviroj P. Naunyn Schmiedebergs. Mechanism of inhibition of catecholamine release from adrenal medulla by diphenylhydantoin and by low concentration of ouabain (10 (-10) M). Arch Pharmacol Feb; 296(3): 293-6. 1977.
10. Leor J, Goldbourt U et al. Digoxin and increased mortality among patients recovering from acute myocardial infarction: importance of digoxin dose, Cardiovasc Drugs Ther, Oct;9(5): 723. 1995.
11. Rathore SS, Curtis JP, Wang Y, Bristow MR, Krumholz HM. Association of serum digoxin concentration and outcomes in patients with heart failure. JAMA. 289(7): 871-8. 19 Feb 2003.
12. Ahmed A, Rich MW, Love TE, Lloyd-Jones DM, Aban IB, Colucci WS, Adams KF, Gheorghiade M. Digoxin and reduction in mortality and hospitalization in heart failure: a comprehensive post hoc analysis of the DIG trial. Eur Heart J. 27(2):178-86. Jan 2006.
13. Vogt AM, Ackermann C, Yildiz M, Schoels W, Kübler W. Lactate accumulation rather than ATP depletion predicts ischemic myocardial necrosis: implications for the development of lethal myocardial injury, Biochim Biophys Acta;1586 (2):219- 26. 16 Mar 2002.
14. Vermeulen RP, et al. Clinical correlates of arterial lactate levels in patients with ST-segment elevation myocardial infarction at admission: a descriptive study. Critical Care 14:R164. 2010.
15. Matsushita K, Williams EK, Mongraw-Chaffin ML, Coresh J, Schmidt MI, Brancati FL, Hoogeveen RC, Ballantyne CM, Young JH. The association of plasma lactate with incident cardiovascular outcomes: The ARIC Study. Am J Epidemiol. 20 Jun 2013.
16. Levy B, Gibot S, Franck P, Cravoisy A, Bollaert PE. Relation between muscle Na+K+ ATPase activity and raised lactate concentrations in septic shock: a prospective study. Lancet 365: 871–75. 2005.
17. Tennant, R. and Wiggers, C.J. The effect of coronary occlusion on myocardial contraction. Am J Physiol 112:351. 1935.
18. Tennant R. Factors concerned in the arrest of contraction in an ischemic myocardial area. Am J Physiol: 133; 677-682. 1935.
19. Cori CF and Cori GT. The mechanism of epinephrine action IV: The influence of epinephrine on lactic acid production and blood sugar utilization. J Biol Chem 84: 683-98. Full text at http://www.jbc.org/content/84/2/683.full.pdf+html. 1929.
20. Williamson JR. Metabolic effects of epinephrine in the isolated, perfused rat heart. J Biol Chem 239: 2721–29 Full text at www.jbc.org/content/239/9/2721.full.pdf 1964.
21. Mercedes Garcia Alvarez, Paul Marik, Rinaldo Bellomo. Stress hyperlactataemia: present understanding and controversy. The Lancet Diabetes & Endocrinology, http://dx.doi.org/10.1016/S22138587(13)70154-2 29 Nov 2013.
22. Yarlioglues M. Kaya MG et al. Dose-dependent acute effects of passive smoking on left ventricular cardiac function in health volunteers. J Investig Med 60 (2): 517-22). Feb 2012.
23. Crawford SO et al. Association of blood lactate with type 2 diabetes: the Atherosclerosis Risk in Communities Carotid MRI Study. Int J Epidemiol. 39(6):1647-55. Dec 2010.
24. Juraschek SP et al. Lactate and Risk of Incident Diabetes in a Case-Cohort of the Atherosclerosis Risk in Communities (ARIC) Study. PLoS ONE 8(1): e55113.doi:10.1371/journal.pone.0055113 www.journals.plos.org/plosone/article?id=10.1371/journal.pone.0055113
25. J Hunter Young, Stephen O Crawford et al. Association of Blood Lactate with Hypertension: The Atherosclerosis Risk in Communities Carotid MRI Study. Circulation: 118:S_1129. 2008.
26. Palmaner G et al. Association of blood lactate with carotid atherosclerosis: The Atherosclerosis Risk in Communities (ARIC) Carotid MRI Study. Atherosclerosis 228 249e255. 2013.
27. Powerpoint slides presented at the King of Organs Conference 2012 and other topics, about the myogenic theory of myocardial infarction, at www.infarctcombat.org/MyogenicTheory.html
28. Mesquita QHde, Baptista CAS. Why Myogenic Theory not Thrombogenic Theory, Arq Bras Cardiol, V. 62 (4), Translated to English at www.infarctcombat.org/MTxTT-ABC.pdf 1994.
29. Mesquita, QHde, Baptista CAS. Cardiotonic: Insuperable in preservation of myocardial stability, as preventive of acute coronary syndromes and responsible for a prolonged survival. Casuistry of 28 years Ars Cvrandi 2002, May 35:3. Translated to English at www.infarctcombat.org/28years/digitalis.html 1972-2000.
30. The effects of cholesterol lowering with simvastatin on cause-specific mortality and on cancer incidence in 20,536 high-risk people: a randomized placebo-controlled trial, Heart Protection Study Collaborative Group. BMC Medicine 2005, 3:6 at www.biomedcentral.com/content/pdf/1741-7015-3-6.pdf
31. Fox KA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome; prospective multinational observation study (Grace). BMJ V 333: 1091-4. 2006.
32. Labout T et al. Predictors and implications of Q-waves in ST-elevation acute coronary syndromes. Am J. Medicine 122(2):144-51. Feb 2009.
33. Lazzarino AI, Hamer M, Gaze D, Collinson P, Steptoe A. The association between cortisol response to mental stress and high-sensitivity cardiac Troponin T plasma concentration in healthy adults. J Am Coll Cardiol. 62(18):1694-1701. 2013.
34. Rob Shave, Aaron Baggish et al. Exercise-Induced Cardiac Troponin Elevation: Evidence, Mechanisms, and Implications. J Am Coll Cardiol 56:169–76). 2010.
35. Wittstein IS et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. New Engl Med J V352 N6. 2005.
36. Gaudreault V et al. Transient Myocardial Tissue and Function Changes During a Marathon in Less Fit Marathon Runners. Canadian J of Cardiology V29 I10. 2013.
37. Opdahl A, Venkatesh BA, Fernandes VRS et al. Resting Heart Rate as Predictor for Left Ventricular Dysfunction and Heart Failure: MESA (Multi-Ethnic Study of Atherosclerosis), J Am Coll Cardiol, 63 (12):1182–9. 2014.
38. Fernandes VRS et al, Subclinical atherosclerosis and incipient regional myocardial dysfunction in asymptomatic individuals. MESA (The Multi-Ethnic Study of Atherosclerosis), J Am Coll Cardiol, 47 (12) : 2420-8. 2006.
Acknowledgement Citation
Stress as Cause of Heart Attacks - The Myogenic Theory first appeared in Wise Traditions in Food, Farming and the Healing Arts, the quarterly journal of the Weston A. Price Foundation, Fall 2014. www.westonaprice.org/modern-diseases/cardiovascular-disease/stress-as-cause-of-heart-attacks/
Comments:
-
Carlos ETB Monteiro said..
Stress as the Major Risk Factor and Coronary Thrombosis as the Consequence of Myocardial infarction.
Some pioneering studies:
1) Selye in 1958 has shown experimentally how stress, combined with some agents, may induce myocardial necrosis where the coronary arteries are perfectly normal. He also said in his paper: “It is noteworthy, however, that, under these circumstances, not only cardiac infarction but organic obstruction of the coronary vessels can regularly be produced by humoral means.” (Hans Selye. The Humoral Production of Cardiac Infarcts, British Medical Journal, March 15: 1958. Full free text at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2028103/pdf/brmedj03094-0021.pdf )
2) Branwwod noticed in 1978 in a study involving one hundred twenty-one patients who had died in a coronary care unit, that the incidence of thrombi was only 35.6% (44 cases). No thrombi were detected in any coronary artery in 64.4% (77 cases). The thrombi and infarct were examined microscopically, and the age of each was correlated according to known criteria. This comparison revealed that of the 44 cases in which occlusive thrombi were detected, the infarct and the thrombus were the same age in 14 cases (32%), while the infarct was older than the thrombus in 30 cases (68%). He told that the factors inducing infarction, apart from hypoxia, were stress, altered cell
membrane permeability, and increased catecholamines. (Branwood AW. The Development of Coronary Thrombosis Following Myocardial Infarction. Lipids V 13 N 5 at http://link.springer.com/article/10.1007/BF02533735 )