Positive Health Online
Your Country

Cognitive Behaviour Therapy
listed in cfs me long covid, originally published in issue 60 - January 2001
|
Foreword Among approaches to the treatment and management of chronic fatigue syndrome (CFS), one of the most controversial is Cognitive Behaviour Therapy or CBT. Many patients with this condition (for whom ME is frequently the preferred title, as CFS appears to underestimate the severity of the symptoms experienced) have expressed concern that CBT is seen in some quarters, particularly among psychiatrists, as a panacea, and the only treatment of any merit.
Editor's Note We think that Positive Health readers should be able to make up their own minds about the use of CBT for patients with ME and we publish the following article, without necessarily endorsing the author's views, in the spirit so as to enable our readers to be better informed about this controversial topic. |
As early as the first century AD, the philosopher, Epictetus, noted that: "Men are disturbed not by things but by the views which they take of them."
Although chronic fatigue syndrome (CFS) is not a psychiatric disorder, mood disturbances are common. Irrespective of what caused the illness, the lack of any definitive prognosis, coupled with the knowledge that there is no recognized cure, causes many patients to suffer considerable anxiety and depression. Moreover, on 'good' days they push themselves to achieve pre-morbid levels of activity, which not only exacerbates their symptoms, but further convinces them of some underlying disease process. Activity is then avoided, the patient becomes preoccupied with symptoms and demoralization sets in, together with an acceptance of life-long illness.[1]
The central tenet of Cognitive Behaviour Therapy (CBT) is the idea that our individual interpretations of life's experiences are beliefs rather than facts. If we hold negative, unrealistic beliefs, emotional upset can result.
One of the main pioneers of CBT was Dr Aaron Beck (1979), and it is from his studies that the principle of cognitive restructuring grew.
A cognition is simply a thought, and Beck showed how the low mood of depressed and anxious people can be improved by altering their thought processes. He called our involuntary thoughts and images 'automatic thoughts', and, left untreated, such dysfunctional thinking becomes a habit. He described how the type of emotion produced depends upon the content of the thought. For example, thoughts of danger give rise to anxiety and panic; thoughts of loss to sadness and depression.
At some time in our lives we all have so-called 'black-and-white' or 'infantile' thinking. When a relationship fails we say we'll never get over it, or we make a serious mistake at work and assume that our career is on the line. In this way, errors of logic occur in our information processing. Beck noted six ways in which this happens:
1. Arbitrary inference – We draw a conclusion regardless of the facts.
Example: 'It's going to rain tomorrow, I've got a day off work.'
2. Selective abstraction – We focus on only one single aspect of a situation.
Example: 'I've got a headache, now the whole day's ruined.'
3. Overgeneralization – We select one or two traumatic experiences and subsequently apply them to every other situation.
Example: 'Neighbours always cause me trouble.'
4. Magnification and minimization – We fail to evaluate the real significance of events and make 'mountains out of molehills', or vice versa.
Example: 'He didn't reply to my invitation, he doesn't like me.'
5. Personalization – We refer unconnected events to ourselves.
Example: 'There's an ambulance! My mother's been taken ill.'
6. Absolutist, dichotomous thinking – This is black-and-white thinking in that events are either viewed as good or bad with no shades of grey.
Example: 'I'm too fat, nobody will ever want to marry me.'
Another psychologist, Albert Ellis, emphasized the role of 'irrational beliefs', such as: 'I should be able to complete this report by tomorrow. If I can't I'm useless.' He identified three major ones:
*I must do well and win people's approval or I'm worthless.
* Other people must treat me as I want them to or they should be punished.
* Life must give me all I want, and nothing I don't want.
|
Table 1 A = Activating event – acute viral infection, stressful life events B = Beliefs C = Emotional consequence – anger, frustration, depression |
In 1977 he put forward his ABC model, which shows the relationship between the way we think and our emotions. CFS is a very individual illness: each sufferer experiences a unique combination of symptoms, and coping strategies are similarly varied. Below, I have applied the Ellis model to my own experiences of the illness.
CBT has become an established treatment for patients attending psychiatric and psychological services for depression, anxiety, phobias, panic disorder and obsessive-compulsive neurosis. More recently, however, the cognitive behavioural approach has been used with patients suffering from CFS.[2]
A cognitive theory of CFS has been developed that tries to explain how certain life stresses can precipitate CFS in predisposed persons, and also how cognitive, physiological, behavioural and social factors then interact to perpetuate the illness (Figure 1).
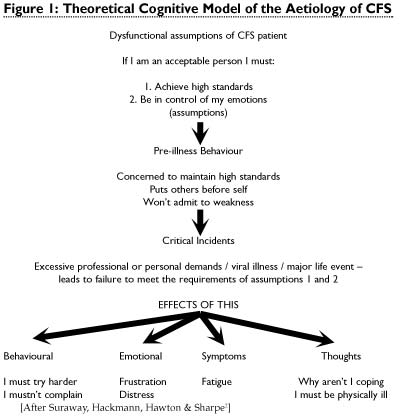
CBT is a form of non-pharmacologic treatment based on a detailed analysis of the patient's thinking and beliefs about their illness. Irrespective of the original physiological cause of the illness, CBT helps to identify the cognitions and behaviours which, in some patients, may be perpetuating symptoms and acting as obstacles to recovery.
Treatment places particular emphasis on helping patients to reappraise their illness beliefs, as well as on increasing activity and solving social and occupational problems where they exist.[3]
On average, patients attend 10-20 one-hour sessions, though some may need long-term treatment and follow-up. Homework assignments are an integral part of treatment.
Although a positive and collaborative relationship between patient and therapist is a prerequisite for effective therapy, this can often be difficult as some patients resist a psychotherapeutic approach.
Table 2 gives a basic outline of what to expect from a whole course and a single session of CBT.
|
Table 2 Outline of a Typical Course of CBT Sessions 1-3 Assessment of the problem Sessions 4-14 Identification of patient's obstacles to recovery – i.e. faulty beliefs and coping behaviours. Sessions 15-16 Consolidation and planning of further self-help Outline of a Single Session: |
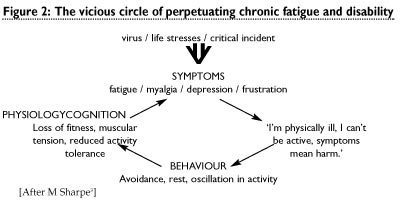
The belief that activity-induced symptoms indicate harm can lead to anxiety and to avoidance of further activity.[3],[4] This, in turn, leads to physiologic changes that increase activity-associated fatigue. When further activity is attempted, the increase in symptoms is even greater than before – confirming the patient's original belief and creating a vicious circle (Figure 2). Trials show that CBT can be particularly effective in enabling patients to break out of this.
Studies have also shown[5] that social and occupational stressors and the beliefs and behaviours of others can perpetuate illness. In my own case this was a very significant factor. Before the onset of my illness I had been suffering prolonged occupational stress, which was later exacerbated when I needed to take long periods of sick leave. As a teacher this meant colleagues often had to lose their free periods to cover my lessons. As I often appeared to be perfectly healthy, this led to further recriminations and emotional abuse. After several years of trying to cope I gave up and applied for ill-health retirement. It's a decision I've often regretted, and one I felt I was forced into, as it's now been shown that, given adequate support from management, it is possible for CFS patients to recover while remaining in employment.
|
Table 3 The main elements of CBT used with CFS patients
[After M Sharpe 3] |
"If workplace rehabilitation is to be attempted it is important that it is co-ordinated with other treatment and rehabilitation measures. If…a programme of CBT is to be undertaken there may be opportunities to ensure that any process of rehabilitation at work is integrated with the therapy programme…dialogue between the occupational physician, employee and others involved in treatment will be of great importance."[6]
"The treatment of CFS requires that the patient is given a positive explanation of the causes of his symptoms, emphasizing the distinction among factors that may have predisposed them to develop the illness (lifestyle, work stress, personality), triggered the illness (viral infection, life events) and perpetuated the illness (cerebral dysfunction, sleep disorder, depression, inconsistent activity, and the misunderstanding of the illness and fear of making it worse)."[6]
How Effective is CBT?
Although it is not a miracle cure, CBT substantially improves the ability of the majority of patients to lead normal lives. There is no other treatment for CFS that has this level of evidence and a number of trials confirm this. In the Oxford Trial[7] around three-quarters of patients receiving CBT had good outcomes at 12 months, compared with only one-quarter who had received medical care alone. Moreover, most of the improvement occurred during the eight months after the course of CBT had ended.
A trial at King's College[8] obtained very similar results. In both trials, improvement was associated with changing the belief that physical activity should be avoided. It is thought, therefore, that this belief may be crucial in perpetuating disability by maintaining avoidance behaviour.
This is further substantiated by two case studies of wheelchair-bound patients.[9]
"At the end of treatment, the patients experienced clinically significant reductions in fatigue, were not using wheelchairs, showed an increase in occupational and social functioning and were leading relatively independent existences."
Gradually, by exploring the patient's fears about her symptoms, the therapist was able to identify her dysfunctional illness beliefs that had resulted in unhelpful coping strategies in the perpetuation of CFS. After 15 months she abandoned her wheelchair and at 21 months had resumed previously stressful and challenging activities.
Although this was an uncontrolled study, it serves to emphasize further the role of dysfunctional beliefs and subsequent coping strategies in the perpetuation of CFS.
It was found that, once successfully engaged in treatment, patients became aware of the psychosocial and personality factors that predispose to and perpetuate their condition. Psychological interventions targeted at challenging illness beliefs and increasing activity significantly improved the well-being of CFS patients.9
Although CBT is clinically proven to be a very effective treatment for many aspects of CFS, it is not well accepted by patient organizations because they think it is too psychological. Moreover, hospitals and health authorities fail to see CFS as a top priority. As a result, very few treatment centres exist and there are not enough trained clinical psychotherapists.
Due to the multi-faceted nature of the illness, practitioners need to take a 'biopsychological' approach to treatment. This is the starting point for CBT-informed practice. Through an empathetic acceptance of the reality of their symptoms, each patient is encouraged towards the view that, although their illness may have been triggered by a physical factor, psychological and social factors may be acting as obstacles to their recovery. CBT teaches patients the coping strategies necessary to overcome these and to break out of the vicious circle of fatigue and disability.
References
1. Suraway C, Hackmann A, Hawton K and Sharpe M. Chronic Fatigue Syndrome: A Cognitive Approach. Behavioural Research Therapy. 33(5): 535-544. 1995.
2. Sharpe M. Psychological Aspects of Chronic Fatigue Syndrome. Bailliere's Clinical Psychiatry. 3(3). 1997.
3. Sharpe M. Cognitive Behaviour Therapy for Chronic Fatigue Syndrome: Efficacy and Implications. The American Journal of Medicine. 105(3A). 1998.
4. Deale A, Chalder T and Wessely S. Illness Beliefs and Treatment Outcome in Chronic Fatigue Syndrome. Journal of Psychosomatic Research. 45(1): 77-83. 1998.
5. Sharpe M, Chalder T, Palmer I and Wessely S. Chronic Fatigue Syndrome, A Practical Guide to Assessment and Management. General Hospital Psychiatry. 19: 185-199. 1997.
6. Mounstephen A and Sharpe M. Chronic Fatigue Syndrome and Occupational Health. Occupational Medicine. 47(4): 217-227.
7. Sharpe M, Hawton KE and Simkin S et al. Cognitive Behaviour Therapy for the Chronic Fatigue Syndrome: A Randomized Controlled Trial. BMJ. 312: 22-26. 1996.
8. Deale A, Chalder T, Marks IM and Wessely S. Cognitive Behaviour Therapy for Chronic Fatigue Syndrome: A Randomized Controlled Trial. American Journal of Psychiatry. 154: 408-414. 1997.
9. Powell P, Edwards RHT and Bentall RP. The Treatment of Wheelchair-Bound Chronic Fatigue Syndrome Patients: Two Case Studies of a Pragmatic Rehabilitation Approach. Behavioural and Cognitive Psychotherapy. 27: 249-260. 1999.
Recommended Reading
Campling F and Sharpe M. CSF/ME The Facts. Oxford University Press. 2000.
This is an inexpensive, practical, self-help guide for patients with CFS/ME. It will be available later this year. £9.99.
Chalder T. Coping with Chronic Fatigue. Sheldon Press. ISBN 0-85969-685-5. 1995.
Available at good bookshops or by mail order to: Sheldon Press Mail Order, 26 Steep Hill, Lincoln LN2 1LU. (£4.99 + £1.00 postage and packing per book.)
The 'Overcoming' series, published by Robinson – £7.99 each. They are essentially self-help guides using cognitive behaviour therapy techniques. Examples include:
Overcoming Depression – ISBN 1841191256
Overcoming Panic – ISBN 1854877011
Overcoming Anxiety – ISBN 1854874225
Overcoming Traumatic Stress – ISBN 1841190160
Overcoming Childhood Trauma – ISBN 1841190801
Overcoming Gambling – ISBN 1854874845
Overcoming Bulimia and Binge Eating – ISBN 1854871714
Overcoming Low Self Esteem – ISBN 1854877259
Overcoming Social Anxiety and Shyness – ISBN 1854877038
Bibliography
Avery B. Principles of Psychotherapy. Thorsons. 1996.
Trower P, Casey A and Dryden W. Cognitive Behavioural Counselling in Action. Sage Publications. 1999.
Acknowledgements
For their invaluable help given in my research for this article, I would like to thank Dr Chris Bass, Dept of Psychological Medicine, John Radcliffe Hospital, Oxford; Dr Michael Sharpe, Dept of Psychiatry, University of Edinburgh; and Professor Simon Wessely, Guys', Kings and St Thomas' School of Medicine.
Editor's Acknowledgement
The Editor is grateful to Dr Derek Pheby for reading the article and providing constructive comment.
Comments:
-
No Article Comments available