Positive Health Online
Your Country

The Real Causes of Heart Disease - [and Statins don't help]
listed in heart, originally published in issue 248 - August 2018
Heart disease is the leading cause of death worldwide. For decades our health authorities and the majority of the medical profession have told us that dietary saturated fat and cholesterol are primary causes of heart disease. This has been the main justification for an estimated thirty-five to forty million people in the United States, seven to eight million people in England, and millions more people worldwide being prescribed cholesterol-lowering statins. However, in this article I will argue that the way we have been looking at the causes of heart disease is fundamentally flawed and taking statins offers very little to no protection.
https://commons.wikimedia.org/wiki/File:Wiki_Heart_Antomy_Ties_van_Brussel.jpg
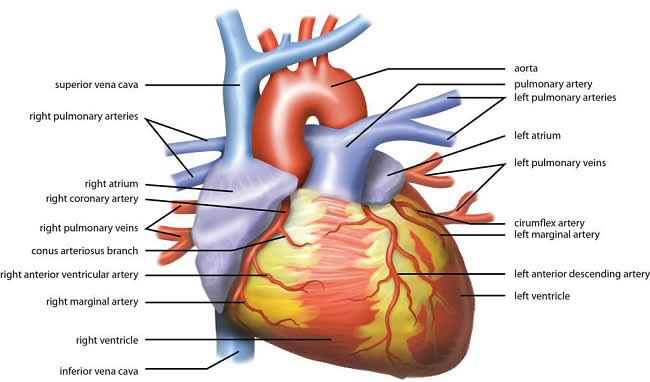
Anatomy of the Heart
Most heart disease is coronary heart disease (CHD), which involves a thickening of the walls of the main arteries that supply blood and oxygen to the heart muscle. The thickening of the arterial wall is accompanied by the formation of blood clots. Eventually blood clots can cause a complete blockage of the artery (occlusion), starving the heart muscle of blood and oxygen, leading to muscle cell death and a heart attack. There is no doubt that heart disease is characterized by a thickening of the artery walls and the formation of blood clots however, these are only some of the important observed features.
https://en.wikipedia.org/wiki/Vascular_smooth_muscle
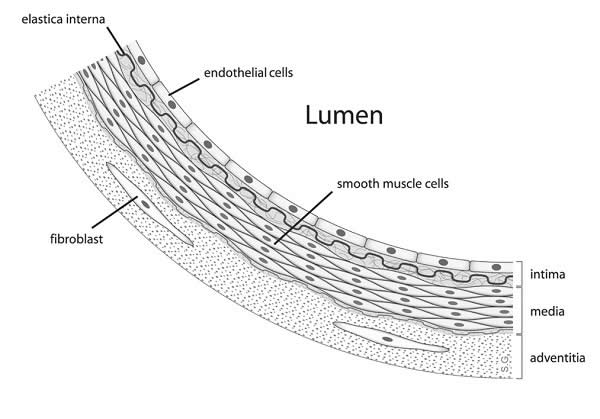
Diagram showing the location of vascular smooth muscle cells
Giorgio Baroldi (1925-2007) was an Italian cardiovascular pathologist who for half a century challenged the conventional theory regarding the processes associated with heart disease. Baroldi made a number of observations that led him to conclude that a blocked artery might not be the most important factor in a heart attack, or at least that the occlusion may not be the only important factor. Baroldi observed that:
- Some people have a significant amount of narrowing of the artery without any signs of damage to the heart muscle itself. And the narrowing could have existed for years without any clinical symptoms of heart disease;
- There is no relationship between the extent of coronary artery disease and the degree of damage to the heart muscle itself. Logically, we would expect that if there were a greater extent of arterial plaque or occlusion, then the area of dead heart muscle tissue would also be greater. However, Baroldi concluded that the extent of arterial disease did not correlate with the degree of actual damage to the heart;
- It is possible to have an infarct (an area of dead heart muscle tissue) without a corresponding occlusion.
In 2004, Baroldi, along with coauthor Professor Malcolm Silver from the University of Toronto, published a book that contains a detailed summary of an alternative view of how heart disease develops.[1] One of the key issues discussed by Baroldi is that in the presence of a blocked artery the heart adapts by increasing blood flow through the collateral circulation. Most people are familiar with illustrations of the gross anatomy of the heart showing the coronary arteries and other anatomical features. However, what is hardly ever shown is the collateral circulation. The collateral circulation consists of an intricate network of smaller blood vessels that also supply the heart muscle with blood and oxygen.
If blocked arteries can be circumvented by the collateral circulation, and there is not a connection between the extent of artery disease and the size of the area of dead heart muscle tissue, then heart attacks could start from within the heart itself rather than as a result of arterial damage. This hypothesis is sometimes referred to as the myogenic theory of myocardial infarction. A pioneer in this field was Dr Quintiliano H. de Mesquita, a Brazilian physician and scientist, whose work has been continued by fellow Brazilian Carlos Monteiro, an independent researcher and scientist.
The myogenic theory raises questions about common surgical procedures that are currently being performed, such as coronary bypass surgery and the insertion of stents. These interventions are based on the idea that a blocked artery will always lead to a heart attack. If that is not the case, then some people might be having costly unnecessary surgical procedures.
The myogenic theory of heart attacks asserts that heart disease is caused by physical and psychological stress that causes a change in the energy systems used by the heart. Despite the fact that we have been told for decades that dietary fat is bad for the heart, fat is in fact the heart’s preferred source of energy. However, when the body’s stress response is activated, the energy producing system that uses glucose is activated, since energy can be derived more quickly from glucose. However, ‘burning’ glucose leaves an acidic byproduct that in turn results in a biochemically more acidic heart muscle.
The acidic environment affects the contractility of the heart muscle. This dysfunction can lead to a localized area of cell death (necrosis).
Once necrosis has occurred and the contractility of an area of the heart muscle is compromised, the fluid dynamics of the arteries changes. This can cause the inside walls of the arteries to become damaged. The body responds to this damage to the arteries by forming blood clots, and the arteries are then subject to various processes associated with the buildup of arterial plaque. If arterial plaque does build up, the resultant narrowing of an artery can make the situation worse by further impeding the supply of blood and oxygen to the heart muscle. The condition will eventually present as arterial plaque, possibly a full occlusion, disruption to the electrical control system of the heart, and an area of dead heart muscle tissue. But what was the main culprit, and which one came first?
There are still a considerable number of unknowns regarding the precise mechanisms involved in the development of heart attacks, and in what order they appear for each individual person. However, even a general wider appreciation of the mechanisms that could be involved can enable better informed choices regarding prevention strategies.
The current model of heart disease basically considers the condition as a simple plumbing problem and focusses on certain risk factors. We have considerable evidence suggesting that the risk factor based approach is much less than complete.
In 2011, a study was published in the Journal of the American Medical Association[2] that should have led to a complete reappraisal of the current risk factor–based approach, but instead it was largely ignored. The study included more than 500,000 people who were admitted to hospital with a first heart attack but without any prior cardiovascular disease. The researchers looked at five of the traditional risk factors in relation to survival after this first heart attack: high blood pressure, smoking, high cholesterol, diabetes, and family history of heart disease. This list of risk factors is similar to those used by the American Heart Association in their cardiovascular risk calculator.
If such risk factors were reliable as predictors of mortality, then we would expect that people with more of them would have worse rates of survival. However, the reverse was true in this study. The more risk factors a person had, the more likely they were to survive their first heart attack. In fact, the greatest risk of death was associated with having no risk factors; people with none of the five risk factors were 1.5 times more likely to die after a heart attack than people who had all five risk factors.
There are many other contradictions to the current model. For example, the fact that people tend to live longer with higher cholesterol levels. This is particularly true in the elderly, where higher cholesterol appears to be protective against heart failure.[3-10]
A study published in the Journal of the American Medical Association analyzed data from 122,458 patients enrolled in fourteen international clinical trials.[11] The researchers compared the frequency of various risk factors in people who had heart disease. They found that only 39 percent of all men and 34 percent of all women who had heart disease had high cholesterol or high triglycerides.
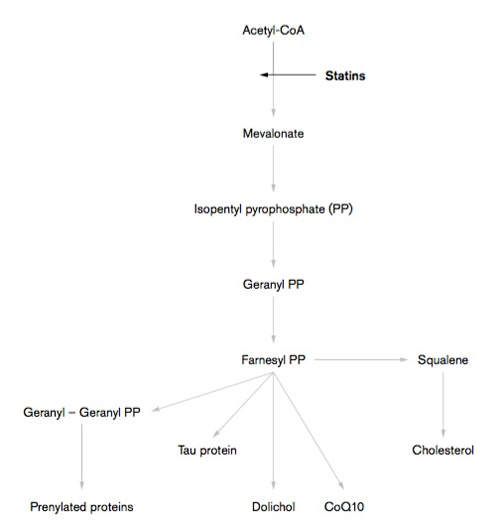
The Mevalonate Pathway and Action of Statins
Cholesterol-lowering statins then, are not the answer. In fact, statins make things worse. Statins are associated with an increase in the amount of arterial plaque.[12-15]
Statins have another detrimental effect on the heart. When we exercise, the heart gets stronger. This adaptation to exercise is important for everyone, and in particular, it is an important part of the recovery process for cardiac patients. Exercise stimulates the body to make more mitochondria, the energy-producing factories within muscle cells. However, statins have been found to block this adaptation.[16]
The Real Causes of Heart Disease
Heart disease is much more complicated than our health authorities would have us believe. We are told that it can be controlled by managing a short list of suggested risk factors - it just so happens that these are the risk factors that medications exist for. In reality, heart disease involves the complex interplay of the stress response, immunity, exercise and other lifestyle factors, the environment, gut health and a wide range of nutritional factors.
Not only do our health authorities mislead us by focusing on suggested risk factors that can be managed by medications. These authorities may outright incorrect statements. For example, the British Heart Foundation[17] states that:
“Stress is not a direct risk factor for cardiovascular disease, but it's possible that it may contribute to your risk level.”
In the rest of this article I would like to introduce some of the reasons why the British Heart Foundation is wrong.
We have already seen above that physical and psychological stress can adversely affect the heart by creating an acidic environment within the heart itself. In addition, excessive stress directly affects the condition of the arteries, the likelihood that blood clots will form, and the electrical system that controls the heartbeat. Stress also ‘burns up’ essential nutrients that would otherwise protect us from heart disease. And stress weakens the immune system such that we can become more vulnerable to infections, which could also play an important role in the development of heart disease.
Stress is of course an individual phenomenon and what one person finds stimulating another person finds stressful. In addition, some people seem to be able to cope with more negative stress than others through a greater capacity to deal with a particular stressor, and excess negative stress manifests as different symptom for different people.
_500x533px.jpg)
Hypothalamus, Pituitary and Adrenal (HPA) Axis – Anterior View
The activation of the stress response causes the release of adrenaline and cortisol. Adrenaline makes the blood more readily able to clot in the case of a physical injury. As we already know, blood clots are an important feature of heart disease.
Adrenaline also affects the heart rate and blood vessels so that cardiac output increases (increasing circulation to the working muscles) - increasing blood pressure. Increased blood pressure could increase the risk of damage to the inside wall of the arteries.
The hormone cortisol has the effect of raising blood glucose levels. Cortisol also contributes to obesity, in particular, central obesity (visceral fat), which has been identified as the more dangerous type of obesity. Overall, changes in blood glucose, increased central obesity, increased blood pressure, and other metabolic changes can increase the risk for type 2 diabetes (T2DM), and people who have T2DM have up to five times the risk of developing heart disease compared to people who don’t have T2DM.
Cortisol has a weakening effect on the immune system, which is one reason why people who are chronically stressed often become more susceptible to infections. Infections could also play a role in heart disease. Cortisol also prevents the body’s cells from losing sodium and encourages the cellular loss of potassium. This imbalance could lead to fluid retention and dysfunction of the cell to the extent that it contributes to heart muscle cell death.
Major stressors can cause a heart attack directly without any existing damage to the arteries or any other risk factors, due to the effects of noradrenaline, which is also released during the stress response. Noradrenaline is released to enable stronger muscle contractions. It is released at nerve endings and can cause bands of cell death (contraction band necrosis).
Stress encourages us to eat poor quality foods and miss out on important heart protective nutrients, as well as to consume more sugar, drink more alcohol, and smoke cigarettes. All of these poor lifestyle choices also impact the balance of the autonomic nervous system, making things worse. In particular, smoking cigarettes further activates the sympathetic nervous system.
Stress also causes Takotsubo cardiomyopathy, also known as broken-heart syndrome, which is a weakening of the heart’s main pumping chamber as a result of severe emotional or physical stress.
However, this is just the tip of the iceberg where stress and its effects on the heart are concerned. Even more profound are the changes in heart rate variability (HRV).
HRV refers to the difference in the time interval between beats of the heart. If the time interval between beats varies a lot, there is a high HRV. One might assume that a predictable, uniform heartbeat (low HRV) is healthy, but in fact the reverse is true. A healthy heart displays a high degree of variability in the beat-to-beat time intervals, as the heart adjusts to whatever demands are placed upon it. A reduced HRV has been shown to predict heart disease death, as well as deaths from all causes.[18-22]
One study published in the Journal of the American College of Cardiology in 2001 followed participants for ten years and found that reduced HRV was associated with more than four times the risk of sudden cardiac death.[20] Another study published in the same journal the same year found that HRV drops even further immediately before a heart attack,[23] noting a gradual decline in HRV starting one hour before a heart attack occurred. The decrease in HRV was even more obvious two minutes before a heart attack, and during the heart attack event itself there was an almost complete withdrawal of vagal activity. The decrease in HRV and the corresponding heart attack were also more closely related to activities associated with mental stress.
In case there is any remaining doubt about stress as a primary cause of heart attacks and death, a study published in the journal Circulation in 2012[24] investigated the use of transcendental meditation for people with heart disease. Participants were split into two groups; one group completed twenty minutes of meditation twice every day, while the other, dubbed the “health education group”, was instructed to spend the same amount of time doing other health-promoting activities such as preparing healthy meals, exercising, or nonspecific relaxation.
After five years of follow-up, 31 percent of the people in the health education group had either had a heart attack or stroke, or died, compared with 20 percent of those in the meditation group, representing an absolute risk reduction of 11 percent associated with meditation, above the benefits associated with more common health-promoting activities.
This study was a secondary prevention trial, which means its participants already had a diagnosis of heart disease at the start of the study. Secondary prevention trials done on statins have shown that statins typically reduce the risk of heart attack and death from all causes by about 1 percent or 2 percent.[25] The data suggests that meditation for twenty minutes twice each day is between five and eleven times more beneficial than taking a statin (depending on which statin clinical trial we use for comparison). Still, leading health authorities maintain that stress is not a cause of heart disease, and instead spend millions on promoting the erroneous cholesterol idea and the widespread use of statins.
References
- Baroldi G, Silver MD. The etiopathogenesis of coronary heart disease: a heretical theory based on morphology. Boca Raton, FL: CRC Press; 2004.
- Canto JG, Kiefe CI, Rogers WJ, et al. Number of coronary heart disease risk factors and mortality in patients with rst myocardial infarction. JAMA 306(19):2120–2127. 2011.
- Krumholz H, Seeman TE, Merrill SS, et al. Lack of association between cholesterol and coronary heart disease mortality and morbidity and all-cause mortality in persons older than 70 years. JAMA: 272(17):1335–1340. 1994.
- Weverling-Rijnsburger AW, Blauw GJ, Lagaay AM, Knook DL, Meinders AE, Westendorp RG. Total cholesterol and risk of mortality in the oldest old. Lancet 350(9085):1119–1123. 1997.
- Krum H, McMurray JJ. Statins and chronic heart failure: do we need a large-scale outcome trial? J Am Coll Cardiol: 39(10):1567–1573. 2002.
- Bohm M, Hjalmarson A, Kjekshus J, et al. Heart failure and statins— why do we need a clinical trial? ZS Kardiologie 94(4):2223–2230. 2005.
- Kjekshus J, Dunselman P, Blideskog M, et al. A statin in the treatment of heart failure? Controlled rosuvastatin multinational study in heart failure (CORONA): study design and baseline characteristics. Eur J Heart Fail.7(6):1059–1069. 2005.
- Cleland JG, Loh H, Windram J, Goode K, Clark AL. Threats, opportunities, and statins in the modern management of heart failure. Eur Heart J. 27(6):641–643. 2006.
- Horwich TB, Hamilton MA, Maclellan WR, Fonarow GC. Low serum total cholesterol is associated with marked increase in mortality in advanced heart failure. J Card Fail. 8(4):216–224. 2002.
- Rauchhaus M, Clark AL, Doehner W, et al. The relationship between cholesterol and survival in patients with chronic heart failure. J Am Coll Cardiol. 42(11):1933–1940 2003.
- Khot UN, Khot MB, Bajzer CT, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 290(7):898–904. 2003.
- Nakazato R, Gransar H, Berman DS, et al. Statins use and coronary artery plaque composition: Results from the International Multi- center Con rm Registry. Atherosclerosis. 225(1):148–153. 2012.
- Raggi P, Davidson M, Callister TQ, et al.. Aggressive versus moder- ate lipid-lowering therapy in hypercholesterolemic postmenopausal women: beyond endorsed lipid lowering with EBT scanning (BELLES). Circulation. 112(4):563–571. doi:10.1161 /CIRCULATIONAHA.104.512681 2005.
- Schmermund A, Achenbach S, Budde T, et al. Effect of intensive versus standard lipid-lowering treatment with atorvastatin on the progression of calci ed coronary atherosclerosis over 12 months: a multicenter, randomized, double-blind trial. Circulation. 113(3):427–437. doi:10.1161/CIRCULATIONAHA.105.568147 2006.
- Saremi R, Bahn G, Reaven PD, et al. Progression of vascular calcication is increased with statin use in the Veterans Affairs Diabetes Trial (VADT). Diabetes Care. 35(11):2390–2392. doi:10.2337 /dc12-0464 2012.
- Mikus CR, Boyle LJ, Borengasser SJ, et al. Simvastatin impairs exercise training adaptations. J Am Coll Cardiol. 62(8):709–714. 2013.
- Stress. Information from BHF website. Accessed 5 June 2018. https://www.bhf.org.uk/heart-health/preventing-heart-disease/stress
- Dekker JM, Schouten EG, Klootwijk P, Pool J, Swenne CA, Kromhout D. Heart rate variability from short electrocardiographic recordings predicts mortality from all causes in middle-aged and elderly men: the Zutphen study. Am J Epidemiol. 145(10):899–908. 1997.
- Huikuri HV, Mäkikallio TH, Airaksinen KE, et al. Power-law relationship of heart rate variability as a predictor of mortality in the elderly. Circulation. 1998;97(20):2031–2036. 1998.
- Mäkikallio TH, Huikuri HV, Mäkikallio A, et al. Prediction of sudden cardiac death by fractal analysis of heart rate variability in elderly subjects. J Am Coll Cardiol. 37(5):1395–1402. 2001.
- Mäkikallio TH, Høiber S, Køber L, et al. Fractal analysis of heart rate dynamics as a predictor of mortality in patients with depressed left ventricular function after acute myocardial infarction. Am J Cardiol. 83(6):836–839. 1999.
- Huikuri HV, Mäkikallio TH, Chung-Kang P, et al. Fractal correlation properties of R-R interval dynamics and mortality in patients with depressed left ventricular function after an acute myocardial infarction. Circulation 101(1):47–53. 2000.
- Kop WJ, Verdino RJ, Gottdiener JS, O’Leary ST, Bairey Merz CN, Krantz DS. Changes in heart rate and heart rate variability before ambulatory ischemic events. J Am Coll Cardiol. 38(3):742–749. 2001.
- Schneider RH, Grim CE, Rainforth MV, et al. Stress reduction in the secondary prevention of cardiovascular disease: randomized, controlled trial of transcendental meditation and health educa- tion in blacks. Circ Cardiovasc Qual Outcomes. 2012;5(6):750–758. doi:10.1161/CIRCOUTCOMES.112.967406.
- Smith J. Statin nation: the great cholesterol cover-up [DVD]. 2012.
Comments:
-
Wendy Musgrave said..
A very interesting read it put a different light on causes of heart disease and how Statins are not that beneficial.
Stress is a main factor in many illnesses in this very hectic life that we all seem to lead nowadays and very hard to control as most of us are on a constant treadmill with work family etc and maybe we should all try to address this and take more time out to relax and be made more aware how beneficial it can be .