Positive Health Online
Your Country

Muscle Energy Techniques (METs) Applied to Knee Pain
listed in bodywork, originally published in issue 191 - February 2012
Introduction
An additional tool for the physical therapist's 'manual therapy toolbox', muscle energy techniques (METs) can help to release and relax muscles, and also stimulate the body's own healing mechanisms. METs are unique in their application, as the client provides the initial effort while the practitioner facilitates the process. The primary force originates from the contraction of soft tissue; this force is then utilised to assist and correct the presenting musculoskeletal dysfunction.
METs are generally classified as direct - as opposed to indirect - techniques because the muscular effort is created from a controlled position and aimed in a specific direction, against a distant counterforce (usually the practitioner). One of the main uses of these methods is to normalize joint range, rather than increase flexibility, and techniques can be used on any joints with restricted range of motion (ROM) identified during the passive assessment.
Benefits of METs
The benefits of METs include:
- Restoring normal tone in hypertonic muscles;
Physical therapists use METs to try to help relax the hypertonic shortened muscles. If a joint has limited ROM, then through the initial identification of the hypertonic structures, appropriate techniques can assist in reaching normality in the tissues. METs applied in conjunction with massage therapy can be very beneficial in helping to achieve this relaxation effect. - Strengthening weak muscles;
METs can be used to help strengthen weak, or even flaccid, muscles: the client is advised to contract the muscle classified as weak against a resistance applied by the therapist (isometric contraction). Timing of techniques can be varied: for example, the client resists the movement to approximately 20 to 30 per cent of their capability for 5 to 10 seconds, rests for 10 to 15 seconds, and then repeats the process five to eight times. This can be improved over time. - Preparing muscle for subsequent stretching;
In some circumstances, the sport in which a client participates may affect joint ROM. Most people can benefit from improved flexibility, and although the focus of METs is to reach 'normal' ROM, a more intensive MET approach can be employed to improve flexibility beyond this. The procedure might involve the client contracting beyond the standard 10 to 20 per cent of the muscle's capability. Once METs have been incorporated into the treatment plan, a flexibility programme could follow. - Improved joint mobility;
One of my favourite sayings when I teach muscle testing courses is: "A stiff joint can become a tight muscle and a tight muscle can become a stiff joint".
Does this not make perfect sense?
When used correctly, METs can improve joint mobility, even when the muscles are relaxing initially. A relaxation period follows the muscle contraction, which then helps to achieve the 'new' ROM.
Main Effects of METs
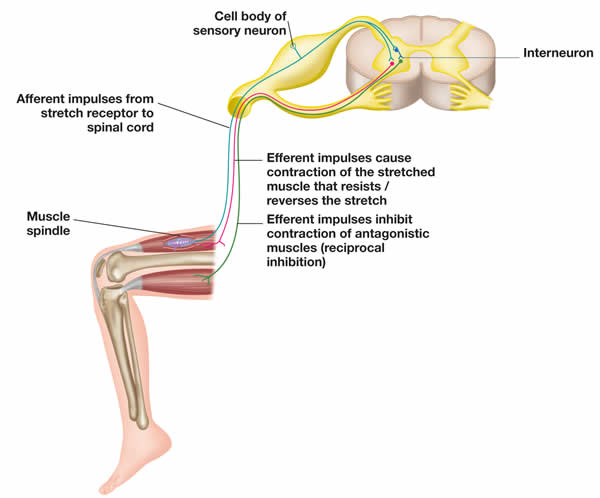
Diagram 1: The stretch reflex arc and reciprocal inhibition (RI)
The main effects of METs can be explained by two distinct physiological processes: post-isometric relaxation (PIR) and reciprocal inhibition (RI). Certain neurological influences occur during METs, but before considering PIR/RI, it is useful to take into account the two types of receptors involved in the 'stretch reflex' (See Diagram 1):
- Muscle spindles sensitive to change in length and speed of change in muscle fibres;
- Golgi tendon organs that detect prolonged change in tension.
Stretching a muscle causes an increase in the impulses transmitted from the muscle spindles to the posterior horn cell (PHC) of the spinal cord. In turn, the anterior horn cell (AHC) transmits a greater number of motor impulses to the muscle fibres, which creates a protective tension to resist the stretch. However, increased tension maintained for a few seconds is sensed within the Golgi tendon organs, which transmit impulses to the PHC and have an inhibitory effect on the increased motor stimulus at the AHC. This inhibitory effect causes a reduction in motor impulses and consequent relaxation.
The net effect is that the prolonged muscle stretch will increase overall stretching capability due to the protective relaxation of the Golgi tendon organs overriding the protective contraction. However, a fast stretch of the muscle spindles will cause immediate muscle contraction and - if not sustained - there will be no inhibitory action.
When an isometric contraction is sustained, neurological feedback through the spinal cord to the muscle itself results in PIR, causing a reduction in tone of the contracted muscle. This lasts for approximately 20 to 25 seconds, during which the tissues can be more easily manipulated to a new resting length.
During RI (Diagram 1), the reduction in tone relies on the physiological inhibiting effect on antagonists during the contraction of a muscle. When the motor neurons of the contracting agonist muscle receive excitatory impulses from the afferent pathway, the motor neurons of the opposing antagonist muscle receive inhibitory impulses from their afferent pathway. It follows that contraction or an extended stretch of the agonist muscle must elicit relaxation or inhibit the antagonist, and that a fast stretch of the agonist will facilitate a contraction of the antagonist. The refractory period also lasts for approximately 20 seconds but, with RI, it is thought to be less powerful than PIR. In certain circumstances, use of the agonist may be inappropriate due to pain or injury.
Method of Treatment
- METs can be used for both acute and chronic conditions, but the intensity and duration of symptoms will determine which variation of MET is suitable;
- The therapist guides the muscle to the point of resistance (point of bind), before releasing slightly from that position (especially if the tissue is tender);
- Against resistance, the client isometrically contracts the affected muscle (PIR) or the antagonist (RI) to approximately 10 to 20 per cent of its strength capabilities;
- The client holds the contraction for 10 to 12 seconds;
- By taking a deep breath in, the client relaxes fully and, as they breathe out, the therapist passively guides the specific joint that lengthens the hypertonic muscle into a new position, effectively normalising joint ROM;
- The process is repeated until no further progress is made (normally three to four times), and the final stretch is held for approximately 20 to 30 seconds.
METs are quite a mild form of stretching when compared to other techniques, such as proprioceptive neuromuscular facilitation (PNF); METs are therefore more appropriate for rehabilitation. Most conditions involving muscle shortening will occur in postural muscles, since they are composed predominantly of slow-twitch fibres, so a milder form of stretching is perhaps more suitable.
Case Study
Sarah, a 35-year-old female, presents with bilateral anterior knee pain, and her right knee is particularly painful. This condition has been present for the last year and has progressively worsened over the last 2 months. Walking up and down stairs, running, sitting for long periods and driving aggravate the knee pain. This patient currently works as a nanny and is constantly bending down to pick up children, but she is finding this simple task very difficult to do because of the pain.
Sarah would like to be able to run a 10km race, but at the moment can only run for about 500m before her pain comes on. It is a constant ache most of the time and she has been given quadriceps exercises by a personal trainer (e.g. squats and leg extensions), but these appear to make matters worse. She also participates in a weekly exercise class but this seems to exacerbate her symptoms too, especially after doing hip-abduction exercises.
After consulting her GP, Sarah was advised to take anti-inflammatory drugs and reduce any exercises that were irritating her knees. The GP also mentioned that because of her pain, she would not be able to participate in any running for the near future. The GP recommended a course of physiotherapy but she is still on the waiting list.
Assessment
With this specific case study, consider what you feel are the 'tissues' that are causing Sarah's pain and the specific condition that might be diagnosed. You might possibly want to jot down the tests that you would conduct, placing an emphasis on the underlying 'cause' of her painful symptoms. (A tip: her knee pain is a weak link in the kinetic chain.)
Let's first look at what Sarah is presenting with. She has bilateral anterior knee pain, which is exacerbated by going up and down stairs, sitting for long periods, etc. In my experience the hypothesis of the diagnosis is that this patient has patellofemoral syndrome (PFS) or simply anterior knee pain. The tissues (which I considered to be responsible for the pain) are around the patellofemoral joint, which is possibly mal-tracking and causing an inflammatory response.
On examination the following tests were positive for the above diagnosis:
- Patella tests (scoop and grinding tests);
- Passive knee flexion with overpressure on the patella causing pain;
- Standing and half squat.
With the above clinical findings I confirmed that it was the patellofemoral joint that was responsible for her pain. The problem with this hypothesis is that patients often expect us to treat the area of pain, which as you will see in this case study will not be the main issue.
There is much literature on the predisposing and pathological causes of PFS: authors write about overpronation, increased Q angle, muscle imbalance, pelvis dysfunction, leg length inequality, etc. My experience of treating PFS considers all of the above factors, but recently I have also had a lot of success with looking at pelvic stability - or rather instability, as is often the case.
The first plan of my assessment was to see if I could change the patient's symptoms by performing a simple technique on the knee. This involved gliding the patella medially while she squatted, which immediately reduced her symptoms. This told me that something was causing the patella to track laterally.
I assessed the tensor fasciae latae (TFL) and iliotibial band (ITB) using Ober's test (see below) and found there was increased tension, especially on the right side. Again, there is another theory that by 'stripping' the ITB, it will release. However, if you think about this logically, why is there increased tension in this structure in the first place? It is more likely trying to stabilize the lateral thigh/knee because structures or muscles are possibly less active. This led me to test the functional ability of the gluteus maximus (Gmax). I would like to explain the functional anatomy of this muscle before I continue with the objective examination.
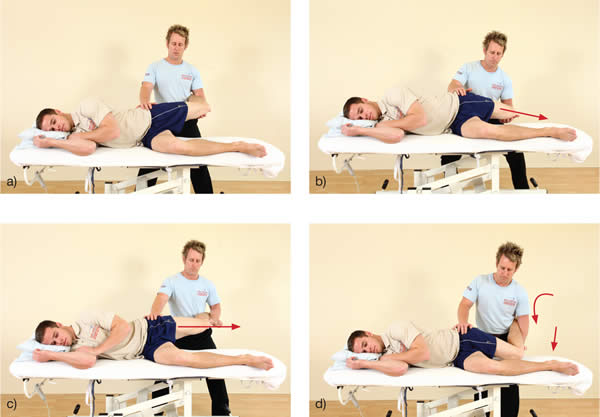
Ober's test. (a) The therapist controls the patient's left knee and asks the patient to relax fully before the knee is lowered towards the couch; (b) The knee dropping down indicates a normal length of TFL/ITB; (c) The knee remaining where it is indicates a tight TFL/ITB; (d) The hip is allowed to 'fall' into hip flexion and internal rotation. One could mistakenly consider the TFL/ITB to be normal length, but a 'tight' TFL/ITB will take the hip into this dysfunctional position.
Gluteus Maximus (Gmax)
The Gmax is a large muscle with a multitude of attachments from the pelvis to the femur. We are taught in our studies that it is a powerful hip extensor, but we might not understand its function during motion. For example, as we step upwards, the Gmax has an external rotation and an abduction influence on the femur to help control the knee alignment, whilst powerful hip extension will propel the body upwards. If the Gmax is weakened, the knee will be observed to deviate medially, which will then predispose the knee to pain.
The patient was tested using the 'prone hip-extension firing pattern test' (see picture below), which confirmed weakness/misfiring in the gluteus maximus muscle.
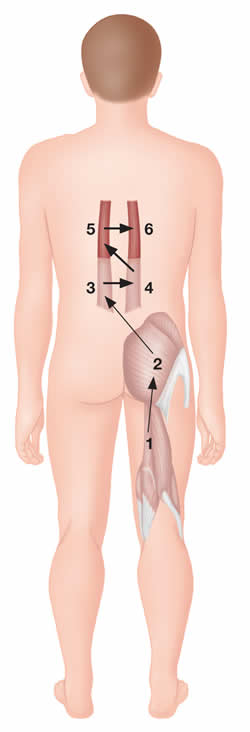
Correct firing pattern of hip joint extension.
Muscle activation sequence
1. Hamstrings - Either group 1 or 2 may normally activate first
2. Gluteus maximus - Either group 1 or 2 may normally activate first
3. Contralateral lumbar extensors
4. Ipsilateral lumbar extensors
5. Contralateral thoracolumbar extensors
6. Ipsilateral thoracolumbar extensors
Another possible cause of the weakness/misfiring in the gluteal group is the opposite muscle group (antagonist) becoming overactive and subsequently being held in a shortened position (hypertonic). This muscle group, if you have not already guessed it, is the psoas and adductor group. If these muscles have become tight, this can contribute to the weakness in the gluteal muscles as a group through neurological inhibition. The psoas and adductor group was functionally tested for apparent length via the Thomas test and was found to be positive bilaterally.

Thomas test. The knee is below the level of the hip, indicating a normal length of the psoas.
Thomas test. The knee is higher than the hip, indicating a tight right psoas. A tight rectus femoris is also seen here.
We also have to take into account the role of the vastus medialis (VM) and its oblique fibres. We know that this muscle has a control function at the knee, as it helps maintain the patella tracking within the trochlear groove of the femur. We are also aware that this muscle becomes inhibited and subsequently atrophies if pain and swelling are present. When this muscle was tested and observed in the patient, it was demonstrated to be weak.
Treatment Plan
The treatment plan involved a simple re-education of the exercises that the patient had already been advised to do, but with a specific focus on technique.
Initially I started treating the patient by using specific METs to promote the lengthening of the psoas, adductors and the TFL/ITB (see the specific METs below).
MET Psoas

The patient flexes their right hip against the therapist's resistance.
The therapist is stabilizing the right hip with their right hand.
The therapist passively extends the hip to lengthen the psoas, assisted by gravity.

From the flexed position, the patient is asked to resist hip flexion.
MET Adductors

The patient adducts their legs.

The therapist lengthens their adductors.
Met TFL / ITB

The patient abducts their right leg.

The patient's left knee is stabilized while the therapist adducts the right leg.
Over the next three weeks, the patient was given a progressive lengthening programme for the psoas, adductors and TFL/ITB. She was also shown some simple re-educating exercises for the control of the Gmax and the VM.
Gmax and VM exercises
The patient adopted a prone position initially to activate the hip-extension exercise to re-educate the firing of the Gmax. She was asked to simply squeeze the Gmax and lift one leg an inch off the floor, then repeat with the opposite leg (perform 12-15 reps for 2 sets).
The second exercise was a half squat using a small step. The patient was advised to bend her knee approximately 10-15 degrees, with the patella being guided towards the second toe to control alignment of the joint. She was then asked to squeeze the inner quad and told to lock the knee into extension, holding for the count of two. This was repeated 10-12 times on each leg for 2 sets. However, this exercise can commonly cause some discomfort to the knee because of general gluteal weakness, incorrect technique, etc. (I have on occasion taped the knee medially while this exercise is performed - this has been shown to reduce the symptoms.)
At each follow-up session, the patient demonstrated a considerable reduction in symptoms, and within six weeks was able to run 5km without any pain. This patient now has no difficulty performing any of her daily tasks within her working environment.
Comments:
-
No Article Comments available