Positive Health Online
Your Country

Headache: Osteopathic Evaluation, Diagnosis and Treatment
listed in osteopathy, originally published in issue 182 - May 2011
Classification of Headaches
There are 5 main classifications of headache:
- Vascular (migraine/cluster/aneurism);
- Tension (muscle contracture);
- Pressure/Inflammatory (brain tumour, infection, cerebrovascular disease,( ICPressure);
- Cranial neuralgias (trigeminal neuralgia;
- Dysfunction of TMJt/assoc muscles);
- Psychotic (usually delusional i.e.; patient "feels worms inside their head" or "bone going rotten").
| Headache Case History Taking Sieve | |
|---|---|
|
Where is the pain?
|
what part of the head, bi/unilateral
|
|
Classic migraine
|
typically unilateral
|
|
Cluster headache
|
unilateral, high on nose behind/over eye
|
|
Acute glaucoma
|
in and around one eye
|
|
Facial sinusitis
|
over frontal or maxillary sinus
|
|
Trigeminal neuralgia
|
check, jaw, lips or gums (2nd/3rd division CNV)
|
|
Giant cell arteritis
|
close to involved artery usually temporal (PMR)
|
|
Headaches from eye disorders will occur around affected eye
|
|
|
What Type of Pain?
|
|
|---|---|
| Aching | most headaches |
| Throbbing | migraine, sinusitis, giant cell arteritis (PMR), meningitis, (throbs & aches) |
| Sharp jabs | trigeminal neuralgia |
|
How Severe is the Pain?
|
|
|---|---|
| Dull ache | tension |
| Severe | cluster, glaucoma, trigem neuralgia, giant cell arteritis, meningitis |
| Very severe | subarachnoid haemorrhage, brain tumour |
| Variable | migraine, toxic (alcohol/drugs), vascular (also throbbing) sinusitis |
What is the duration?
How long have they had it?
|
What is the Onset?
|
|
|---|---|
| Gradual | tension, eye disorders, chronic subdural heamatoma; |
| Gradual but getting worse and does not tend to respond to medication | brain tumour; |
| Rapid | migraine, cluster, glaucoma, trigeminal neuralgia, meningitis, subarachnoid haemorrhage |
|
What is the frequency / How long does it last?
|
|
|---|---|
| Weeks to months | tension, post concussion syndrome |
| Hours to days | migraine, meningitis, subarachnoid haemorrhage |
| Hours | cluster, sinusitis |
| Seconds to minutes | trigeminal neuralgia |
|
Is it acute or chronic and re-occurring?
|
|
|---|---|
| Acute | subarachnoid haemorrhage, meningitis, toxic vascular (alcohol/drugs) |
| Chronic | tension, migraine, cluster |
|
If chronic, has it changed its characteristics or become progressively severe?
|
|
|---|---|
| Progressively more severe | chronic subdural heamatoma, brain tumour |
| Tends to diminish | post concussion syndrome |
|
Does the Pain Occur at the Same Time every Day?
|
|
|---|---|
| Daily pattern | sinusitis, hypertension (worse am improves when upright), cluster |
Does coughing and sneezing or changing the position of the head affect the headache?
Yes sinusitis, brain tumour, post concussion syndrome
Yes cervical disc prolapse/irr to grt occipital nerve (C2)
|
Painful Structures in the Head
|
|
|---|---|
| Intracranial | Extracranial |
| Venous sinuses | Scalp vessels |
| Cortical veins | Scalp muscles |
| Basal arteries | Orbital contents |
| Dura of anterior, middle & posterior fossa | Mucus membranes-para/nasal spaces External and middle ear Teeth and gums |
With structures above the tentorium cerebelli, pain pathways travel via the trigeminal nerve and are therefore perceived in the frontal, temporal & parietal regions of the head. For structures below the tentorium cerebelli pain pathways travel via the glossopharyngeal / vagus nerves and upper cervical spinal nerve roots and pain is perceived mainly in the occipital region (Ward, 2000).
Examination
- Active / passive movements of the cervical spine/temporomandibular joint;
- Compression test;
- Blood pressure;
- Eye/vision examination.
- Neurological examination including relevant cranial nerve testing;
- Tap over frontal and maxillary sinuses (if you suspect sinusitis);
- Kernig's sign (if you suspect meningitis);
- Vertebro basilar insufficiency.
Red Flags
- Severe pain - subarachnoid haemorrhage, giant cell arteritis, meningitis
- Visual changes - glaucoma, giant cell arteritis (PMR), space occupying lesion
- Associated fever, sore throat and neck stiffness - meningitis
- Associated fever, malaise, anorexia, muscular aches and stiffness, tenderness of scalp - giant cell arteritis
- Alterations of consciousness - chronic subdural heamatoma, subarachnoid haemorrhage
- Neurological symptoms - chronic subdural heamatoma, brain tumour
- NB: If you suspect any of the above then the patient must be referred immediately
Structural Osteopathic Approach to the Treatment of Migraine of Biomechanical Origin
Classification
- Trigger Factors causing a Migraine Headache
- Chemical toxins
- Various E numbers
- Red wine
- Cheese
- Chocolate,
- Bright light.
With the exception of the latter these all have a direct effect on the carotid arteries and ultimately the flow of blood to the brain (Davidoff RA 1995); however, there are also a number of indirect mechanisms, which involve the biomechanics of the cervical spine.
Physiology of Migraine from a Biomechanical Perspective
Irritation to the cervical sympathetic plexus can be caused by a number of factors namely whiplash injury, anterior osteophytes formation, disc prolapse and over sprain to the anterior longitudinal ligament, with associated shortening to longus coli muscle. This combination can result in compression and over stimulation of the cervical sympathetic plexus (Bowles 1993), causing excess sympathetic discharge, resulting in vasoconstriction of the carotid arteries. This is usually noted by the patient as the aura phase (Penderson DM 1991). Excess sympathetic discharge cannot continue indefinitely and eventually it peaks and then abruptly stops. This allows the para sympathetics, to work unopposed causing vasodilatation of the carotid arteries (Moskowitz MA 1984). This reduces the blood, flow to the brain and resultant ischaemia of neural tissue and pain, ensues.
Osteopathic intervention can be to work on the longus coli muscle through soft tissue and MET techniques to reduce pressure on the cervical sympathetic plexus thereby reducing potential irritation, along with correcting dysfunction of the cervical and thoracic spine through manipulation.
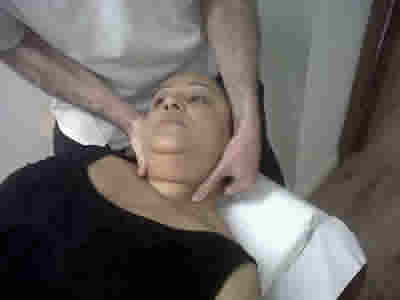
Soft tissue Techniques to longus coli
Patient Position
Patient supine head and neck supported to avoid extension.
Procedure 1
- With the operator standing at the head of the couch.
- Using finger pads of caudad hand palpate anterior to the articular pillar of the cervical spine and lateral to sterno-cleido-mastoid (SCM)
- With the operators cephalad hand placed gently on the patient's forehead, start to rotate the head left if allowing the right SCM to relax and visa versa. This gains improved access to left longus coli.
- Using a gentle cross-fibre type action the left middle fibres of longus coli are drawn towards the midline.
- Continue to repeat until change in the muscle is felt. Do not over do and observe patients facial expressions at all times. Remember the vital structures in this area.

Cross fibre to longus coli.
Procedure 2 Lower fibres of longus coli
- 1. Patient remains supine. The operator rotates the head fully to the right to place their thumb under SCM and anterior to the cervical articular pillar.
- 2. Gentle downward pressure is then placed on the middle fibres of longus coli. This creates a false origin.
- 3. The operator then introduces side bending left while continuing to place pressure on the right longus coli.This creates a longitudinal stretch to the lower fibres of the muscle.
- 4. Repeat until a change is felt in the muscle. Again do not over do sidebending.
Longitudinal stretch to the lower fibres of longus coli.
Management Plan
- Once a diagnosis of classical migraine is made the follow should be considered
- Examination of cervical/thoracic spines identification of joint restriction dealt with by articulation, MET or HVT according to the tissue state.
- Palpation of soft tissue i.e. longus coli sub occipital regions assessed for hypertonia and dealt with through soft tissue / MET techniques accordingly.
- Adaptation of patient activities/ergonomics/diet through advice to prevent repetitive migraine episodes, thereby improving patient's day-to-day activities.
References
Bowles DB. Visual field effects of classical migraine Brain & Cognition 21:181-183. 1993.
Davidoff RA. Trigger factors and non pharmacological approaches Migraine, Manifestations and Management. 183-189. 1995.
Kidd RF. Musculoskeletal dysfunction of the neck in migraine and tension headache Headache, 33(10): 566-569. 1993.
Pederson DM. Migraine aura without headache Journal of Family Practice 32:5-7. 1991.
Greenman PE. Principles of manual medicine. 2nd Edition. Lippincott Williams and Wilkins. Baltimore, USA. 1996.
Stone C. Science in the art of osteopathy. 1st edition. Nelson Thornes Ltd, UK. 1999.
Thomas J., Monaghan T. Clinical examination and practical skills. 1st Edition Oxford University Press, UK. 2007.
Ward RC. et al. Foundations for Osteopathic Medicine. 2nd edition. Lippincott Williams and Wilkins, Baltimore, USA. 2002.
Comments:
-
Carol Daniels said..
Since having the occipital nerve stimulator trial the right side of my brain, scalp and right ear feels light it is under water. I have had my ears checked and no problem. What is my recorse?
-
David Lintonbon said..
Dear Carol,
Have you had the area examined by an osteopath? You may have a problem with the occipito-atlantal joint causing a reflex tightening of the sub-occipital muscles and compression of the underlying occipital nerve.
If you would like to discuss this further please email me on: dlintonbon@hotmail.com
www.theartofhvt.com