Positive Health Online
Your Country

Letters to the Editor Issue 280
listed in letters to the editor, originally published in issue 280 - August 2022
Medical Profession should better Appreciate that Uncertainty Requires Open-Minded Thought
Edwin Salter MA MSc PhD
Recently (Positive Health Online 269) I argued that the huge curriculum of medical training is both wasteful and impairing of practice. One result of this over-burdening is a simplifying closure of thought. “A pill for every ill” (recent criticism added by Stephen Powis of NHS England) is an example of this damage and expense. The doctor listens (alas the Covid telephone consultation) for a symptom word associated with a familiar disorder and promptly writes the usual prescription.
Appropriate are reminders of medical 'authority' resistant even to simple and obviously effective change. A famous historical example is that of Semmelweiss, hounded for imposing hand-washing to prevent spread of childbed fever. Modern examples include prehabilitation (as in pre-op fitness) long ignored because of its military and sport origins, and the surgical checklist, again resisted for supposed negative implication and origin in another discipline (ergonomics).
With an ageing population, an increasing problem is mental and physical damage after surgery. Is the problem with the anaesthetic (choose 'local' if possible) or the surgical damage and body response (promoting a positive rather than fearful context might help)? The two effects can be separated for research and treatment, but inertia obstructs. The widespread resistance encountered by antibiotics (complacently overprescribed for many years, also for livestock) requires an urgent major rethink (consider phages, non-pill methods of administration, other competition examples in biology).
It should be said that there is much in the 'alternative and complementary' field open to similar criticism. Treatments enthusiastically advocated but never of much use have just vanished, and some continue (homeopathy supported by placebo effects?) without facing decisive test (“seems of benefit” needs confirmation as by adequate blind, controlled, experiment). But general medicine is so important to us all that it must not evade scrutiny.
The medical profession should better appreciate that uncertainty requires open-minded thought. And might 'Suggestions' boxes abound for patient input?
Edwin Salter MA MSc PhD <kl.humanfactors@talktalk.net>
Monkeypox Infection – To Fear or Not to Fear?
Commentary by Thomas E Levy MD JD
As of the writing of this article, multiple news reports have recently addressed the occurrence of monkeypox virus infections in humans. In the current setting of the entire planet dealing with the COVID pandemic over the last two and a half years, fear is readily stoked that another pandemic with a virus that comes from the same family of viruses as smallpox could be poised to inflict widespread suffering and death. This article will present the significant scientific data and literature surrounding monkeypox infection in humans, which clearly demonstrates that the monkeypox virus presents NO threat of a pandemic or even a large epidemic.
Monkeypox Characteristics
Although many have never heard of it until recently, monkeypox infection is not the result of the emergence of a new virus. Rather, it was first identified in captive cynomolgus monkeys in Denmark in 1958. [1] The first documented human infection was reported in 1970 in a 9-month-old in the Congo. After clinically recovering from the infection and its associated rash over a month-long period, this baby then contracted the measles and died six days later. [2] While not found exclusively in remote populations in Central and West Africa, limited monkeypox outbreaks appear to have occurred most commonly in such areas of the world, where advanced malnutrition can potentially make some otherwise benign infections life-threatening. [3] This initial case also serves to highlight the fact that underlying chronic malnutrition with moderate to severely depleted vitamin and mineral stores in those living in such remote areas of Africa literally sets the stage for contracting any infectious disease. Quickly contracting measles upon the resolution of the monkeypox virus is the logical result of such an advanced depletion of nutrients in the body. The typical mild to moderate clinical presentation of the measles can easily evolve into a fatal infection when a chronic state of nutrient depletion is still further depleted by a month-long bout with the monkeypox virus.
Monkeypox cases have only occurred as very limited outbreaks, never as an epidemic or a pandemic. Such an outbreak is a cluster of cases in a given area from a pathogen with a limited contagion risk. An epidemic/pandemic requires a pathogen that is very easily spread. This is not the case with the monkeypox virus. The United States has already had an outbreak of monkeypox infection in 2003, involving 47 human cases felt to be secondary to the importation of infected wild rodents from Ghana. No secondary larger outbreak or epidemic resulted, however. Furthermore, no human-to-human transmission was documented. [4] Typically, while human-to-human transmission is certainly possible, it is the exposure to and/or the consumption of infected animals, as well as their consumption of each other, that both spreads this virus and serves as a reservoir for it. This is an additional reason for its primary presence in Africa, in addition to the overall poor nutrition on much of this continent. [5,6]
Monkeypox is characterized as a zoonotic infection, meaning it can transmit from animal to human, or vice-versa. [7] Asymptomatic monkeypox infections are very common, as over half of the healthy persons in an area of Ghana, which actually had no reported clinical human cases of monkeypox at the time of this study, had positive immunoglobulin G (IgG) antibodies against the monkeypox virus genus. [8] A similarly large percentage of the healthy residents in a region of the Congo had circulating antibodies as well. [9] Another study in Cameroon found these antibodies in slightly over a third of the subjects tested. [10] This indicates that monkeypox is not typically severe in its clinical course, much less fatal, in any human population. And this would especially be the case in the United States or in a comparable country with a relatively high-quality level of nutrition as well as a relatively widespread intake of vitamin and mineral supplementation.
Ebola, another virus that has been largely limited to African countries, resulted in a substantial outbreak in West Africa from 2014 to 2016, but it never approached pandemic or even significant epidemic proportions. Nevertheless, in the nutrition-depleted populations in which it emerged, death resulted in those individuals demonstrating clinical infection between 25% and 90% of the time, enough to generate a great deal of fear that it could spread and kill easily throughout the world. [11] And even though Ebola killed many who became infected, a substantial number of those individuals exposed developed natural immunity (IgG antibody) response without ever becoming clinically ill. Depending on the location of the African community and the conditions of the testing protocol itself, up to 50% of exposed individuals, including those living with clinically infected individuals, showed the development of natural antibodies to Ebola without ever becoming ill. [12-18] And in spite of the initial fear that was generated, no pandemic, epidemic, or even minor outbreak of Ebola ever occurred in the United States, even though international airline travel reliably introduced infected individuals into the country. [19,20]
Most of the fear currently seen with the potential spread of the monkeypox virus is due to the fact that both monkeypox and smallpox comes from the same genus of DNA viruses. [21] Smallpox has been estimated to have killed between 300 and 500 million people in the 20th century. [22] Understandably, then, anything that is remotely related to smallpox can be expected to generate a great deal of concern.
While the smallpox vaccine is credited for the effective eradication of smallpox, it is also believed by some that waning vaccine immunity is currently leaving over 70% of the world's population unprotected against smallpox, as this vaccine has not been routinely administered since 1980. [23] Some estimates indicate that the smallpox vaccination has offered roughly an 85% protection against monkeypox infection. [24] And since the vaccine immunity against smallpox is felt to be waning, the associated cross-immunity against related viruses like monkeypox is felt to be fading as well. [25]
However, monkeypox is simply not smallpox. The evidence presented above indicates that many asymptomatic infections occur with monkeypox, and that it is far less contagious than smallpox, with human-to-human transmission being decidedly uncommon. Concurrent epidemics or outbreaks of smallpox and monkeypox have not been reported, and smallpox is not a zoonotic infection like monkeypox, but infects humans only. [26]
Finally, in the more well-fed and healthy populations in the world, monkeypox is simply not a killer virus once contracted. The typical clinical course of monkeypox in such populations much more resembles chickenpox than smallpox. Even if the presumed waning protection of the old smallpox vaccinations results in some increase in human monkeypox cases, it will not turn monkeypox into the highly contagious and deadly killer that is smallpox.
Easily Prevented, Readily Resolved
While some viruses are much more contagious and much more capable of causing severe illness and even death than others, they all share therapeutic susceptibilities. As devastating as Ebola has been to many of the individuals in Africa who have contracted it, bio-oxidative treatment readily resolves it as well as any other virus that is treated before too much advanced organ damage has already taken place. At the height of the Ebola scare in 2014, Drs Robert Rowen and Howard Robins were so convinced of their ability to cure Ebola infections that they put themselves directly in harm's way by traveling to Sierra Leone, a West African epicentre of Ebola infection at that time. Of note, many physicians and other healthcare providers in this area of Africa were dying from the infection at that time.
The primary therapy they used to treat the Ebola patients was ozone. And even though great local resistance was met in gaining access to patients, four individuals were successfully treated with ozone therapy. The cornerstone ozone application was direct intravenous ozone gas injection. Supplemental oral vitamin C therapy was administered as well to address its infection-induced deficiency, to bolster immune function, and to minimize the impact of any possible pro-oxidant Herxheimer-like rapid virus kill-off reactions. All four patients improved immediately after the first treatment and complete resolution of their infections was seen between two to five days. Furthermore, no progression of any Ebola-related symptoms was seen after the first ozone treatments were administered. [27]
Other acute viral syndromes that have initially had much of the world on edge in recent years have also been proven to be readily curable, although not with any known prescription drugs. In 2014, Chikungunya virus received a lot of attention, and some outbreaks with this virus were sizeable, although never really reaching epidemic proportions. This viral infection typically left those infected with debilitating symptoms, often resulting in severe pain in many of the joints in the body. The most immunocompetent individuals would often resolve their most severe symptoms in about a week, but in some the joint pain would become chronic and last as long as five years. Separate one-time intravenous infusions with two bio-oxidative agents (vitamin C and hydrogen peroxide) in 56 patients were highly effective in both completely resolving this viral infection, as well as in immediately alleviating much of the chronic pain that remained long after the acute phase of the infection. [28] Treatment with just high-dose vitamin C intravenously (as much as 100 grams daily) in the acute stage of viral infection with Chikungunya, influenza, Zika, and dengue has also been reported to be similarly curative. [29-32]
In a nutshell, unless the patient has advanced organ damage and is very near death, intravenous vitamin C, in sufficient doses, can always be expected to save the patient from succumbing to an advanced infection, especially viral. As the primary electron-donating nutrient in the body, enough vitamin C must be administered to both neutralize the new, ongoing infection-derived pro-oxidants (toxins) while restoring (reducing) the physiological function of those biomolecules that have already been oxidized. A sizeable number of integrative medicine practitioners who appreciate the therapeutic value of IV vitamin C remain needlessly wary of 50- to 100-gram infusions of vitamin C. This unnecessary caution too often results in a total daily dose of vitamin C of 25 grams or less that proves insufficient to save the patient with severe and widespread oxidative damage secondary to an advanced infection. Nevertheless, even such lower doses can oftentimes suffice, just not as reliably so.
The experience at the Riordan Clinic alone in Wichita, Kansas clearly establishes the safety (and efficacy) of even the highest dosing regimens of vitamin C on a routine basis. Over the past 32 years, over 150,000 intravenous infusions of vitamin C have been administered at Riordan campuses. Doses have varied from 7.5 to 250 grams daily, with 50 grams being the most common dose administered. NO significant adverse side effects have occurred, and NO kidney stones have resulted. For more information on the vitamin C-related research and results of the Riordan Clinic, see: https://riordanclinic.org/journal-articles/.
The primary bio-oxidative therapies (vitamin C, hydrogen peroxide, ozone, ultraviolet blood irradiation, and hyperbaric oxygen) have all been shown to eradicate any viral infections for which they have been properly administered. As noted above, intravenous ozone can promptly resolve even an advanced viral infection whenever access to it is available. Properly-dosed intravenous hydrogen peroxide is comparably effective, and as long as the healthcare practitioner is willing to use it, its expense is nominal and it is available literally everywhere. Vitamin C, ultraviolet blood irradiation, and hyperbaric oxygen therapy are incredibly effective as well, but less available and anywhere from slightly to substantially more expensive to apply than the hydrogen peroxide and/or the ozone therapies. These therapies, along with other supportive antipathogenic measures, are discussed in greater detail elsewhere. [33]
Another great option for dealing with any virus once contracted is a combination vitamin C-cortisol approach, especially when the intravenous administration of bio-oxidative agents is not readily available, if at all. A sizeable oral dose of vitamin C (3 to 5 grams, liposome-encapsulated or as sodium ascorbate powder) along with 20 mg of cortisol (hydrocortisone) is dramatically effective in its clinical impact, often resulting in a prompt cessation of infection evolution followed shortly thereafter by complete resolution. As a very general guideline, the vitamin C/cortisol should be taken three times daily until baseline health is restored. Complete clinical resolution is typically seen in 12 to 36 hours. A more prolonged treatment plan is only required when the pathogen has had a longer time to replicate and clinical illness is more pronounced when therapy is initiated. [34,35]
Recap
Monkeypox virus should never be confused with smallpox, even though the viruses have some common family roots. Smallpox is a human infection, and monkeypox is primarily limited to infections in susceptible animal populations. When monkeypox does infect a human, its clinical course is little more than that of a typical case of chickenpox, as long as the infected individual is not grossly malnourished. And even in populations with significant nutrient depletion, monkeypox is very often a completely asymptomatic infection, as high levels of protective antibodies to monkeypox have been documented in significant percentages of these populations. Also, unlike smallpox, monkeypox has both a very low level of contagion and only rarely results in a fatal outcome, even in the most susceptible of populations.
A good level of nutrition, along with judicious supplementation with vitamins and minerals, will almost completely prevent the transmission of monkeypox, from either an infected animal or human. And when it is contracted, the application of any of a number of bio-oxidative and other therapies will give a rapid resolution to this infection. This ease of prevention and susceptibility to rapid cure should be kept in mind before deciding to proceed directly with any monkeypox vaccinations that end up being offered to the public.
References
- Magnus P, Andersen E, Petersen K, Birch-Andersen A (1959) A pox-like disease in cynomolgus monkeys. Acta Pathologica, Microbiologica, et Immunologica Scandinavica 46:156-176.
- Ladnyj I, Ziegler P, Kima E (1972) A human infection caused by monkeypox virus in Basankusu Territory, Democratic Republic of the Congo. Bulletin of the World Health Organization 46:593-597. PMID: https://pubmed.ncbi.nlm.nih.gov/4340218
- Beer E, Rao V (2019) A systematic review of the epidemiology of human monkeypox outbreaks and implications for outbreak strategy. PLoS Neglected Tropical Diseases 13:e0007791. PMID: https://pubmed.ncbi.nlm.nih.gov/31618206
- Reynolds M, Davidson W, Curns A et al. (2007) Spectrum of infection and risk factors for human monkeypox, United States, 2003. Emerging Infectious Diseases 13:1332-1339. PMID: https://pubmed.ncbi.nlm.nih.gov/18252104
- Ye F, Song J, Zhao L et al. (2019) Molecular evidence of human monkeypox virus infection, Sierra Leone. Emerging Infectious Diseases 25:1220-1222. PMID: https://pubmed.ncbi.nlm.nih.gov/30900976
- Patrono L, Pleh K, Samuni L et al. (2020) Monkeypox virus emergence in wild chimpanzees reveals distinct clinical outcomes and viral diversity. Nature Microbiology 5:955-965. PMID: https://pubmed.ncbi.nlm.nih.gov/32341480
- Eltvedt A, Christiansen M, Poulsen A (2020) A case report of monkeypox in a 4-year-old boy from the DR Congo: challenges of diagnosis and management. Case Reports in Pediatrics 2020:8572596. PMID: https://pubmed.ncbi.nlm.nih.gov/32328334
- Reynolds M, Carroll D, Olson V et al. (2010) A silent enzootic of an orthopoxvirus in Ghana, West Africa: evidence for multi-species involvement in the absence of widespread human disease. The American Journal of Tropical Medicine and Hygiene 82:746-754. PMID: https://pubmed.ncbi.nlm.nih.gov/20348530
- Lederman E, Reynolds M, Karem K et al. (2007) Prevalence of antibodies against orthopoxviruses among residents of Likouala region, Republic of Congo: evidence for monkeypox virus exposure. The American Journal of Tropical Medicine and Hygiene 77:1150-1156. PMID: https://pubmed.ncbi.nlm.nih.gov/18165539
- Guagliardo S, Monroe B, Moundjoa C et al. (2020) Asymptomatic orthopoxvirus circulation in humans in the wake of a monkeypox outbreak among chimpanzees in Cameroon. The American Journal of Tropical Medicine and Hygiene 102:206-212. PMID: https://pubmed.ncbi.nlm.nih.gov/31769389
- Nyakarahuka L, Kankya C, Krontveit R et al. (2016) How severe and prevalent are Ebola and Marburg viruses? A systematic review and meta-analysis of the case fatality rates and seroprevalence. BMC Infectious Diseases 16:708. PMID: https://pubmed.ncbi.nlm.nih.gov/27887599
- Baxter A (2000) Symptomless infection with Ebola virus. The Lancet 355:2178-2179. PMID: https://pubmed.ncbi.nlm.nih.gov/10881884
- Mulangu S, Borchert M, Paweska J et al. (2016) High prevalence of IgG antibodies to Ebola virus in the Efe' pygmy population in the Watsa region, Democratic Republic of the Congo. BMC Infectious Diseases 16:263. PMID: https://pubmed.ncbi.nlm.nih.gov/27286990
- Mafopa N, Russo G, Wadoum R et al. (2017) Seroprevalence of Ebola virus infection in Bombali District, Sierra Leone. Journal of Public Health in Africa 8:732. PMID: https://pubmed.ncbi.nlm.nih.gov/29456826
- Mbala P, Baguelin M, Ngay I et al. (2017) Evaluating the frequency of asymptomatic Ebola virus infection. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences 372:20160303. PMID: https://pubmed.ncbi.nlm.nih.gov/28396474
- Timothy J, Hall Y, Akoi-Bore J et al. (2019) Early transmission and case fatality of Ebola virus at the index site of the 2013-2016 West African Ebola outbreak: a cross-sectional seroprevalence survey. The Lancet. Infectious Diseases 19:429-438. PMID: https://pubmed.ncbi.nlm.nih.gov/30799252
- Bratcher A, Hoff N, Doshi R et al. (2021) Zoonotic risk factors associated with seroprevalence of Ebola virus GP antibodies in the absence of diagnosed Ebola virus disease in the Democratic Republic of Congo. PLoS Neglected Tropical Diseases 15:e0009566. PMID: https://pubmed.ncbi.nlm.nih.gov/34383755
- Manno D, Ayieko P, Ishola D et al. (2022) Ebola virus glycoprotein IgG seroprevalence in community previously affected by Ebola, Sierra Leone. Emerging Infectious Diseases 28:734-738. PMID: https://pubmed.ncbi.nlm.nih.gov/35202536
- Fairley J, Kozarsky P, Kraft C et al. (2016) Ebola or not? Evaluating the ill traveler from Ebola-affected countries in West Africa. Open Forum Infectious Diseases 3:ofw005. PMID: https://pubmed.ncbi.nlm.nih.gov/26925428
- Rauch S, Jasny E, Schmidt K, Petsch B (2018) New vaccine technologies to combat outbreak situations. Frontiers in Immunology 9:1963. PMID: https://pubmed.ncbi.nlm.nih.gov/30283434
- Babkin I, Babkina I, Tikunova N (2022) An update of orthopoxvirus molecular evolution. Viruses 14:388. PMID: https://pubmed.ncbi.nlm.nih.gov/35215981
- Muhlemann B, Vinner L, Margaryan A et al. (2020) Diverse variola virus (smallpox) strains were widespread in northern Europe in the Viking Age. Science 369:eaaw8977. PMID: https://pubmed.ncbi.nlm.nih.gov/32703849
- Rao A, Schulte J, Chen T et al. (2022) Monkeypox in a traveler returning from Nigeria-Dallas, Texas, July 2021. MMWR. Morbidity and Mortality Weekly Report 71:509-516. PMID: https://pubmed.ncbi.nlm.nih.gov/35389974
- Fine P, Jezek Z, Grab B, Dixon H (1988) The transmission potential of monkeypox virus in human populations. International Journal of Epidemiology 17:643-650. PMID: https://pubmed.ncbi.nlm.nih.gov/2850277
- Simpson K, Heymann D, Brown C et al. (2020) Human monkeypox-after 40 years, an unintended consequence of smallpox eradication. Vaccine 38:5077-5081. PMID: https://pubmed.ncbi.nlm.nih.gov/32417140
- Grant R, Nguyen L, Breban R (2020) Modelling human-to-human transmission of monkeypox. Bulletin of the World Health Organization 98:638-640. PMID: https://pubmed.ncbi.nlm.nih.gov/33012864
- Rowen R, Robins H, Carew K et al. (2016) Rapid resolution of hemorrhagic fever (Ebola) in Sierra Leone with ozone therapy. African Journal of Infectious Diseases 10:49-54. https://www.ajol.info/index.php/ajid/article/view/126773
- Marcial-Vega V, Gonzalez-Terron G, Levy T (2015) Intravenous ascorbic acid and hydrogen peroxide in the management of patients with Chikungunya. Boletin de la Asociacion Medica de Puerto Rico 107:20-24. PMID: https://pubmed.ncbi.nlm.nih.gov/26035980
- Gonzalez M, Miranda-Massari J, Berdiel M et al. (2014) High dose intravenous vitamin C and Chikungunya fever: a case report. Journal of Orthomolecular Medicine volume 29. https://isom.ca/wp-content/uploads/High-Dose-Intraveneous-Vitamin-C-and-Chikungunya-Fever-A-Case-Report-29.4.pdf
- Gonzalez M, Berdiel M, Miranda-Massari J et al. (2016) High dose intravenous vitamin C treatment for Zika fever. Journal of Orthomolecular Medicine volume 31. https://isom.ca/wp-content/uploads/High-Dose-Intravenous-Vitamin-C-Treatment-for-Zika-Fever-31.1.pdf
- Gonzalez M, Berdiel M, Duconje J et al. (2018) High dose intravenous vitamin C and influenza: a case report. Journal of Orthomolecular Medicine volume 33. https://isom.ca/article/high-dose-vitamin-c-influenza-case-report/
- Miranda-Massari J, Toro A, Loh D et al. (2021) The effects of vitamin C on the multiple pathophysiological stages of COVID-19. Life 11:1341. PMID: https://pubmed.ncbi.nlm.nih.gov/34947872/
- Levy T (2021) Rapid Virus Recovery: No need to live in fear! Chapter 10. Henderson, NV: MedFox Publishing. Free download available here: https://www.rvr.medfoxpub.com/
- Levy T (2021) http://orthomolecular.org/resources/omns/v17n28.shtml
- Levy T (2022) http://orthomolecular.org/resources/omns/v18n06.shtml
The views presented in this article are the author's and not necessarily those of all members of the Orthomolecular Medicine News Service OMNS Editorial Review Board.
Nutritional Medicine is Orthomolecular Medicine
Orthomolecular medicine uses safe, effective nutritional therapy to fight illness. For more information: www.orthomolecular.org
Find a Doctor
To locate an orthomolecular physician near you:
http://orthomolecular.org/resources/omns/v06n09.shtml
The peer-reviewed Orthomolecular Medicine News Service is a non-profit and non-commercial informational resource.
Editorial Review Board
Albert G. B. Amoa, MB.Ch.B, Ph.D. (Ghana)
Seth Ayettey, M.B., Ch.B., Ph.D. (Ghana)
Ilyès Baghli, M.D. (Algeria)
Ian Brighthope, MBBS, FACNEM (Australia)
Gilbert Henri Crussol, D.M.D. (Spain)
Carolyn Dean, M.D., N.D. (USA)
Ian Dettman, Ph.D. (Australia)
Susan R. Downs, M.D., M.P.H. (USA)
Ron Ehrlich, B.D.S. (Australia)
Hugo Galindo, M.D. (Colombia)
Martin P. Gallagher, M.D., D.C. (USA)
Michael J. Gonzalez, N.M.D., D.Sc., Ph.D. (Puerto Rico)
William B. Grant, Ph.D. (USA)
Claus Hancke, MD, FACAM (Denmark)
Tonya S. Heyman, M.D. (USA)
Patrick Holford, BSc (United Kingdom)
Suzanne Humphries, M.D. (USA)
Ron Hunninghake, M.D. (USA)
Bo H. Jonsson, M.D., Ph.D. (Sweden)
Dwight Kalita, Ph.D. (USA)
Felix I. D. Konotey-Ahulu, MD, FRCP, DTMH (Ghana)
Jeffrey J. Kotulski, D.O. (USA)
Peter H. Lauda, M.D. (Austria)
Alan Lien, Ph.D. (Taiwan)
Homer Lim, M.D. (Philippines)
Stuart Lindsey, Pharm.D. (USA)
Pedro Gonzalez Lombana, MD, MsC, PhD (Colombia)
Victor A. Marcial-Vega, M.D. (Puerto Rico)
Juan Manuel Martinez, M.D. (Colombia)
Mignonne Mary, M.D. (USA)
Jun Matsuyama, M.D., Ph.D. (Japan)
Joseph Mercola, D.O. (USA)
Jorge R. Miranda-Massari, Pharm.D. (Puerto Rico)
Karin Munsterhjelm-Ahumada, M.D. (Finland)
Tahar Naili, M.D. (Algeria)
W. Todd Penberthy, Ph.D. (USA)
Zhiyong Peng, M.D. (China)
Isabella Akyinbah Quakyi, Ph.D. (Ghana)
Selvam Rengasamy, MBBS, FRCOG (Malaysia)
Jeffrey A. Ruterbusch, D.O. (USA)
Gert E. Schuitemaker, Ph.D. (Netherlands)
Han Ping Shi, M.D., Ph.D. (China)
T.E. Gabriel Stewart, M.B.B.CH. (Ireland)
Thomas L. Taxman, M.D. (USA)
Jagan Nathan Vamanan, M.D. (India)
Garry Vickar, M.D. (USA)
Ken Walker, M.D. (Canada)
Anne Zauderer, D.C. (USA)
Andrew W. Saul, Ph.D. (USA), Editor-In-Chief
Associate Editor: Robert G. Smith, Ph.D. (USA)
Editor, Japanese Edition: Atsuo Yanagisawa, M.D., Ph.D. (Japan)
Editor, Chinese Edition: Richard Cheng, M.D., Ph.D. (USA)
Editor, French Edition: Vladimir Arianoff, M.D. (Belgium)
Editor, Norwegian Edition: Dag Viljen Poleszynski, Ph.D. (Norway)
Editor, Arabic Edition: Moustafa Kamel, R.Ph, P.G.C.M (Egypt)
Editor, Korean Edition: Hyoungjoo Shin, M.D. (South Korea)
Editor, Spanish Edition: Sonia Rita Rial, PhD (Argentina)
Contributing Editor: Thomas E. Levy, M.D., J.D. (USA)
Contributing Editor: Damien Downing, M.B.B.S., M.R.S.B. (United Kingdom)
Assistant Editor: Helen Saul Case, M.S. (USA)
Technology Editor: Michael S. Stewart, B.Sc.C.S. (USA)
Associate Technology Editor: Robert C. Kennedy, M.S. (USA)
Legal Consultant: Jason M. Saul, JD (USA)
Comments and media contact: drsaul@doctoryourself.com OMNS welcomes but is unable to respond to individual reader emails. Reader comments become the property of OMNS and may or may not be used for publication.
Acknowledgment Citation
Click here to see a web copy of this news release: https://orthomolecular.acemlna.com/p_v.php?l=1&c=241&m=240&s=c7ae1002d2f579a22c16a1b89c854212
Childhood Obesity Increases Risk of Type 1 Diabetes
Being overweight in childhood increases the risk of developing type 1 diabetes in later life, according to the findings of a new study that analysed genetic data on over 400,000 individuals. The study, co-led by researchers from the Universities of Bristol and Oxford and published in Nature Communications,[1] also provides evidence that being overweight over many years from childhood influences the risk of other diseases including asthma, eczema and hypothyroidism.
The number of individuals being diagnosed with type 1 diabetes has increased drastically in the last 20 years. One possible explanation is the rising prevalence of childhood obesity in an increasingly obesogenic environment. Poor diets with high fat, salt and carbohydrate may compromise early life health-promoting effects of the bacteria in the gut and pancreatic beta-cell fragility in childhood and subsequently increase type 1 diabetes risk.
In contrast to type 1 diabetes, there is irrefutable evidence that children who are overweight are more likely to develop type 2 diabetes and that weight loss can lead to its sustained remission. However, detecting reliable evidence for the factors that contribute to type 1 has been challenging, particularly given that individuals are typically diagnosed early in life before reaching adulthood.
Researchers analysed human genetic data from 454,023 individuals from the UK Biobank and 15,573 type 1 diabetes cases from other cohorts and applied a scientific technique called Mendelian Randomization (MR) to provide evidence that childhood adiposity increases type 1 diabetes risk. As an individual’s genetic alleles are fixed at birth, MR is typically more robust to confounding factors than conventional epidemiological studies. Furthermore, when adiposity differs between individuals, then whether that difference is due to environmental influences (such as diet or exercise) or is due to genetic influences will not change the increased disease risk caused by adiposity. This means that inferences regarding the consequences of obesity on disease risk from MR studies can be more reliable than from conventional observational studies. The authors of this study have pioneered a recent advancement in the field using MR to separate the independent contributions of adiposity at distinct time points in life (i.e. during childhood and adulthood).
By applying this technique, the study’s findings support the inference that greater adiposity in early life increases the risk of type 1 diabetes among individuals and that the increasing prevalence of childhood obesity likely contributes to the rising numbers of type 1 diabetes cases. For comparative purposes, the team also investigated the consequences of childhood adiposity on other diseases with an immune component, such as asthma, eczema and hypothyroidism. They show, that whilst childhood obesity increases risk of these other diseases, this is likely due to a long-term consequence of being overweight for many years over the life course.
Dr Tom Richardson, a Research Fellow at Bristol’s MRC Integrative Epidemiology Unit and Bristol Medical School’s Population Health Sciences, and the study’s lead author, said:
“The effect of childhood obesity directly increases type 1 diabetes risk, emphasizing the importance of implementing preventative policies to lower the prevalence of childhood obesity and its subsequent influence on the rising numbers of cases for this lifelong disease.
“A critical window exists in childhood to mitigate the influence of adiposity on the escalating numbers of type 1 diabetes diagnoses. A 22 per cent reduction in the number of these cases is plausible if the proportion of children within the highest obesity category were to be reduced by ten per cent, from 15.9 to 5.9 per cent. This will help ease healthcare burdens and also potentially improve the quality of life for individuals living with this lifelong disease.”
The study was funded by the Medical Research Council (MRC), the JDRF and Wellcome.
Reference
- Richardson, T.G., Crouch, D.J.M., Power, G.M. et al. Childhood body size directly increases type 1 diabetes risk based on a lifecourse Mendelian randomization approach. Nature Communications 13, 2337 . https://doi.org/10.1038/s41467-022-29932-y 2022.
Further Information
About Type 1 Diabetes
Type 1 diabetes is a serious condition where your blood glucose (sugar) level is too high because your body can’t make a hormone called insulin.
This happens because your body attacks the cells in your pancreas that make the insulin, meaning you can’t produce any at all. We all need insulin to live. It does an essential job. It allows the glucose in our blood to enter our cells and fuel our bodies.
When you have type 1 diabetes, your body still breaks down the carbohydrate from food and drink and turns it into glucose. But when the glucose enters your bloodstream, there’s no insulin to allow it into your body’s cells. More and more glucose then builds up in your bloodstream, leading to high blood sugar levels. (Source: Diabetes.org.uk)
About Mendelian Randomization
Information on Mendelian Randomization: a method of using variation in genes of known function between people to examine the causal effect of a modifiable exposure (i.e., diet) on disease (i.e. cancer) in observational studies. The use of genetics reduces any potential measurement or human, error associated with questionnaires and participant recall which are often used to record lifestyle factors such as level of physical activity. We have published guides in the BMJ and Nature Reviews Methods, contributed to bmj and freakonomics podcasts, and produced a two-minute video primer.
Source and Further Contact
For further information, to arrange an interview with the researchers, or a copy of the paper, please contact Mon/Tues press-office@bristol.ac.uk, [Weds to Fri], Caroline Clancy, Media Manager, email: caroline.clancy@bristol.ac.uk , Mmobile: +44 (0)7776 170238 in the University of Bristol Media & PR Team.
Issued by the University of Bristol Media Team. Caroline.Clancy@bristol.ac.uk
New Study Links Gut Microbiota Strains with more Severe Strokes
A new study has identified strains of gut microbiota that are associated with more severe strokes and worse post-stroke recovery, revealing that the gut microbiome could be an important factor in stroke risk and outcomes.[1]
The study, presented at the European Stroke Organisation Conference (ESOC 2022) pinpointed specific groups of bacteria associated with poorer neurological recovery from ischaemic stroke both in the acute phase (24 hours) and after three months.
The research identified multiple types of bacteria were associated with ischemic stroke risk, including Fusobacterium and Lactobacillus. Negativibacillus and Lentisphaeria were associated with a more severe stroke in the acute phase (at 6 and 24 hours respectively) and Acidaminococcus related to poor functional outcomes at three months.
Dr Miquel Lledós, lead author from the Sant Pau Research Institute Stroke Pharmacogenomics and Genetics Laboratory, Barcelona, Spain, commented
“The influence of the gut microbiome – the trillions of bacteria and other microorganisms that live in the gut – is a modifiable risk factor associated with the risk of stroke and with post-stroke neurological outcomes. However, most research has previously been done in animal models.”
“In this study we took faecal samples – the first samples taken after the event – from 89 humans who’d suffered an ischaemic stroke. Comparing with a control group, we were able to identify multiple groups of bacteria that were associated with a higher risk of ischaemic stroke.”
An ischaemic stroke occurs when a clot or other blockage blocks the blood supply to the brain and is the most common type of stroke. In Europe, 1.3 million people suffer a stroke every year and it is the second most common single cause of death.[2]
“The discovery opens the exciting prospect that, in the future, we may be able to prevent strokes or improve neurological recovery by examining the gut microbiota. In other pathologies, clinical trials are being carried out where researchers replace the intestinal flora through dietary changes or faecal transplantation from healthy individuals and this should be studied further in the stroke field.”
The association between certain strains of gut bacteria and risk of ischaemic stroke was reinforced in another study presented at ESOC this week by a team from Yale University, Connecticut, USA.[3]
The researchers analysed statistics from the Flemish Gut Flora Project and the MEGASTROKE consortium, using a technique called Mendelian Randomisation (MR) which measures variation in genes to examine the causal effect of an outcome or exposure. The study identified 20 microbial traits significantly associated with the risk of developing at least one subtype of ischaemic stroke.
Four Facts on Stroke
- In 2017, there were 1.12 million first strokes in the EU, 9.53 prevalent stroke cases and 460,000 stroke-related deaths;[4]
- In 2017, there were 7.06 million disability adjusted years lost due to stroke in the EU;[4]
- By 2047 it has been estimated there will be an additional 40,000 strokes per year in the EU (a rise of 3%);[4]
- 80% of premature heart disease and stroke is preventable.[5]
References
- Influence of the gut microbiome in ischemic stroke risk and ischemic stroke outcome, presented at the European Stroke Organisation Conference, 4 May 2022.
- Status and Perspectives of Acute Stroke Care in Europe | Stroke (org)
- The gut microbiome influences the risk of acute ischemic stroke: a Mendelian randomization study, presented at the European Stroke Organisation Conference, 5 May 2022.
- https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.029606
- https://www.euro.who.int/en/health-topics/noncommunicable-diseases/cardiovascular-diseases/data-and-statistics
About the Study Author
Dr Miquel Lledós is from the Sant Pau Research Institute Stroke Pharmacogenomics and Genetics Laboratory, Barcelona, Spain.
About ESO
The European Stroke Organisation (ESO) is a pan-European society of stroke researchers and physicians, national and regional stroke societies, and lay organizations, founded in December 2007. The ESO is an NGO comprised of individual and organizational members. The aim of the ESO is to reduce the burden of stroke by changing the way that stroke is viewed and treated. This can only be achieved by professional and public education and making institutional changes. ESO serves as the voice of stroke in Europe, harmonizing stroke management across the whole of Europe and taking action to reduce the burden.
Contact and Further Information
For more information or to arrange an expert interview, please contact Luke Paskins or Sean Deans on luke.paskins@emotiveagency.com, sean.deans@emotiveagency.com or press@eso-stroke.org, or Tel: +44 (0) 208 154 6396.
Media Source
ESOC 2022 Press Team <press@eso-stroke.org >
Sarcopenic Obesity Linked to Dementia in Elderly Patients
Dementia is a major health condition that affects over 15% Japanese people aged over 65 years. There are many reasons for the onset of dementia, among which sarcopenic obesity is considered a higher risk factor for various cognitive impairments. Does this association exist with dementia too? In this new study, a group of researchers from Japan addresses this question. They establish the association between sarcopenic obesity and dementia, opening up new possibilities in dementia treatment.
Obesity, an increasingly prevalent lifestyle disease, often occurs along with poor muscle mass. This condition, called sarcopenic obesity, is evaluated based on the patients’ body mass index (BMI) and handgrip strength. Interestingly, sarcopenic obesity is known to increase the risk of cognitive impairment. Dementia, a cognitive condition where memory, thinking and social abilities progressively decline, is known to significantly affect the quality of life in elderly people. Is this condition associated with sarcopenic obesity?
In a new study published in Clinical Nutrition, a group of researchers led by Dr. Yoshifumi Tamura of Juntendo University, Japan, explored this very question.[1]
“If the association between sarcopenic obesity and dementia is established, appropriate preventive measures can be taken to reduce the occurrence of this condition and the risk of dementia in elderly patients,” says Dr Tamura, stressing on the importance of their study.
This study was made available online on March 16, 2022 and was published in Volume 41 Issue 5 of the Journal on May 01, 2022. www.clinicalnutritionjournal.com/article/S0261-5614(22)00091-7/fulltext
In the study, the researchers recruited 1615 older Japanese adults aged 65 to 84 years participating in the Bunkyo Health Study. The researchers divided the subjects into four groups based on their sarcopenia and obesity status: those with obesity, those with sarcopenia, those with sarcopenic obesity, and those without obesity or sarcopenia (control). They studied the link between various mental processes, sarcopenia, and obesity status. Sarcopenia or poor muscle strength was determined based on a handgrip strength of less than 28 kg in men and 18 kg in women, while obesity status was given to patients with a BMI greater than 25 kg/m2. Two assessment methods were performed to establish the presence of mild cognitive impairment (MCI) and dementia. A score of less than 22 points on the Montreal cognitive assessment and less than 23 points on the Mine-Mental State Examination were used to confirm MCI and dementia respectively.
They found that 59.4% of the population had neither obesity nor sarcopenia, 21.2% had obesity, 14.6% had sarcopenia, and 4.7% of the population had sarcopenic obesity. The participants with sarcopenic obesity had the greatest rate of MCI and dementia, followed by those with sarcopenia, obesity, and finally the control group. When the team ran multivariate analyses to check for statistically relevant associations, they found that sarcopenic obesity was independently associated with an increased prevalence of MCI and dementia compared with the absence of sarcopenia and obesity. The study also showed that sarcopenia is significantly associated with dementia in women, but not in men.
“This study clearly demonstrates that sarcopenic obesity, defined by the combination of BMI and hand grip strength is associated with MCI and dementia among Japan’s elderly people,” says Dr Tamura.
But what are the long-term implications of this study?
Dr Tamura’s answer to this question is encouraging.
“Since we now know that there is a strong correlation between sarcopenic obesity and dementia, we may develop new treatment methods to manage the condition, thereby even reducing the prevalence of dementia.”
Reference
- Yuki Someyaa, Yoshifumi Tamuraa, b, Hideyoshi Kagab, Daisuke Sugimotob, Satoshi Kadowakib, Ruriko Suzukib, Shigeki Aokia, c, Nobutaka Hattoria, d, Yumiko Motoia, e, Kazunori Shimadaa, f, Hiroyuki Daidaa, f, Muneaki Ishijimaa, g, Kazuo Kanekoa, g, Shuko Nojirih, Ryuzo Kawamoria, b, Hirotaka Watadaa, b. Sarcopenic obesity is associated with cognitive impairment in community-dwelling older adults: The Bunkyo Health Study. Clinical Nutrition 41 (5): 1046-1051. 01 May 2022. DOI: https://doi.org/10.1016/j.clnu.2022.03.017
Author Affiliations:
aSportology Center, Juntendo University Graduate School of Medicine, Tokyo, Japan
bDepartment of Metabolism & Endocrinology, Juntendo University Graduate School of Medicine, Tokyo, Japan;
cDepartment of Radiology, Juntendo University Graduate School of Medicine, Tokyo, Japan;
dDepartment of Neurology, Juntendo University Graduate School of Medicine, Tokyo, Japan;
eDepartment of Diagnosis Prevention and Treatment of Dementia, Juntendo University Graduate School of Medicine, Tokyo, Japan;
fDepartment of Cardiovascular Medicine, Juntendo University Graduate School of Medicine, Tokyo, Japan;
gDepartment of Medicine for Orthopaedics and Motor Organ, Juntendo University Graduate School of Medicine, Tokyo, Japan;
hMedical Technology Innovation Center, Juntendo University, Tokyo, Japan.
About Dr Yoshifumi Tamura
Yoshifumi Tamura is an Associate Professor at the Department of Metabolism & Endocrinology, Juntendo University Graduate School of Medicine in Tokyo, Japan. Also affiliated to the university’s Sportology Center, he also served as the former councilor of Japan Sports Agency. Prof Tamura’s research topics include insulin resistance, clinical diabetology, exercise therapy, and sarcopenia. He has published over 83 papers and articles.
Source and Further Information
Brijesh Manek <brijesh.manek@cactusglobal.com>
Original Press Release: https://en.juntendo.ac.jp/news/nid00001481.html
Hospital Study Shows that Covid-19 Can be Prevented with Hydrogen Peroxide
by Albert GB Amoah MD PhD, Seth Ayettey MD PhD, Thomas E Levy MD JD, and Richard Z Cheng MD PhD
Daily mouth rinse, gargle and nasal rinse with dilute hydrogen peroxide solution can prevent Covid-19.
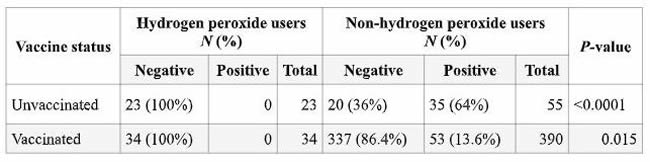
In a recent study, over 4,000 patients and 89 healthcare staff of a hospital in Ghana used hydrogen peroxide on a daily basis during the peak season of Covid-19 season (April 2021 - Dec 2021). None of the 4,000+ patients got Covid-19. None of the 89 staff got Covid-19, except one who discontinued the use of hydrogen peroxide! [1] In another hospital during the same period, out of 424 staff who were fully vaccinated, 34 used hydrogen peroxide and did not develop Covid-19, but 53 didn't use hydrogen peroxide and developed Covid-19. This is statistically significant. Out of the 78 unvaccinated staff, 23 used hydrogen peroxide and none of them got Covid-19. Of the remaining 55 unvaccinated who did not use hydrogen peroxide, 35 got Covid-19. This is statistically significant. These results suggest that even vaccines are not as effective as hydrogen peroxide in the prevention of Covid-19.
The Covid-19 virus (SARS-Cov-2) and other respiratory viruses invade our body through the nose and the mouth. This study shows for the first time that we can stop and kill these viruses in the mouth and nose before they invade deeper into our lungs and the blood stream to cause severe clinical symptoms using hydrogen peroxide.
This study shows that 1% hydrogen peroxide mouth wash and gargle, and 0.5% hydrogen peroxide for nasal cavity rinse (2-3 large drops per nostril) once daily was enough to significantly reduce the risks of Covid-19. [1] The table below from the report summarizes part of the results. In the video below, we have discussed and explained the significance of this study, including safety issues of hydrogen peroxide: https://www.brighteon.com/76f0c65b-69e9-4023-a2a8-0c31e72af047
Table 1. Coronavirus disease 2019 status and use of hydrogen peroxide in unvaccinated and vaccinated healthcare workers at Shai-Osudoku District Hospital in Ghana from April 1 to December 31, 2021
Hydrogen Peroxide History
Hydrogen peroxide is a well-known antiseptic, used extensively in dentistry and to disinfect surfaces and instruments. But many are unaware that hydrogen peroxide is a natural molecule that exists everywhere in the body, including in the immune/defensive cells that have very important biological functions to protect the body from disease.
Hydrogen peroxide was discovered over 200 years ago in 1818, and in 1856 it was found to be present in the human body. In 1888, hydrogen peroxide was reported for the first time to be effective for treating numerous diseases, including scarlet fever, diphtheria, nasal catarrh, acute coryza (rhinitis), whooping cough, asthma, hay fever and tonsillitis. It was also used as an oral and nasal antiseptic in the1918 Spanish flu pandemic.
In the 1960s, hydrogen peroxide was found to have a protective effect on myocardial ischemia. Intravenous infusion of hydrogen peroxide has been studied and promoted for the treatment of various diseases including cancer, skin diseases, polio and bacteria-related mental illness, even in pain relief.[2]
Dr. Levy's book "Rapid Virus Recovery" is on the use of hydrogen peroxide to prevent and treat viral infections, and has over 600 citations. [3] It reviews and analyzes the safety, effectiveness, biological mechanisms and the potential practical uses of hydrogen peroxide.
Hydrogen peroxide (HP) is an inexpensive, safe, and effective over-the-counter topical agent when taken as a mouthwash or when nebulized. [4-7] Knowing the availability of this natural agent and its practical utility may protect us from the current and future unknown viral infections involving the respiratory tract.
Moving Forward
The Covid-19 pandemic swept through and turned the entire world upside down with a virus that was previously unknown. Without specific drugs and vaccines for this virus (SARS-Cov-2), the world panicked and as a result millions of lives and billions upon billions of dollars were lost.
We share this world with many microorganisms including bacteria and viruses, some of which can cause human diseases. Despite the human stockpile of antibiotics for bacterial infections, there are very few antiviral drugs. There is currently no fail-proof medication that is effective against coronavirus diseases encountered so far including MERS (Middle East Respiratory Syndrome) and SARS (Severe Acute Respiratory Syndrome) and several other viral infections. Antiviral drugs and vaccines specific to a new virus take a long time to develop. As we have witnessed first-hand, Covid-19 vaccines took a year to roll out, setting a world record. Even then, after being fully vaccinated, several booster doses are required to prevent severer forms of COVID-19.
The Covid pandemic is not over yet, and epidemics and pandemics appear to be on the rise. [8] We believe that everyone should consider these questions:
- What have we learned from the global management of the Covid-19 pandemic?
- Are we prepared for the next epidemic/pandemic?
- When the next epidemic/pandemic hits, what are you going to do?
- What about other known viral infections, such as the common cold and viral pneumonia?
- Are there safe and effective remedies?
If the word is spread about the effectiveness of hydrogen peroxide in preventing severe viral infections of the respiratory tract including the lungs, very likely we can avoid a future pandemic of such diseases.
Panel Members:
Host: Richard Z. Cheng, M.D., Ph.D. is an NIH-trained and board certified American anti-aging physician. Dr. Cheng is also an inductee of the Orthomolecular Medicine Hall of Fame. [9]
Dr. Albert G.B. Amoah, Former vice dean, University of Ghana Medical School. Author of the HP clinical report. [1] Emeritus Professor of Medicine and Therapeutics and a Consultant Physician at the University of Ghana. He holds the MB;ChB degree from University of Ghana and PhD degree from the University of Surrey, UK. Among his distinguished achievements is the setting up of a National Diabetes Management and Research Center, a center of excellence for multi-disciplinary diabetes care, training and research in Ghana. He has a membership of the Royal College of Physicians (UK) and fellowships of the West Africa College of Physicians, the Ghana College of Physicians and the Ghana Academy of Arts and Sciences.
Dr. Seth Ayettey, Professor and former dean, University of Ghana Medical School. Author of the HP clinical report. [1] Graduated MB; ChB from the University of Ghana Medical School in 1974 and PhD from Cambridge University in 1978. He served as Chair of the Department of Anatomy at the University of Ghana Medical School from 1981 to 1997, Dean of that school from 1998 till 2000, and first Provost of the College of Health Sciences, University of Ghana from 2000 to 2004. He taught Anatomy for 37 years, retiring 2015. Four years of his teaching and research life were spent at the Tulane University Medical Center as a Visiting Professor. Dr. Ayettey has contributed a great deal to knowledge of the structural basis for the excitation-contraction coupling in the specialized and the general myocardium of the mammalian heart. His recent effort, together with his team in Ghana, has been in researching hydrogen peroxide protection against COVID-19. Dr. Ayettey is also a pastor of the Presbyterian Church of Ghana. Three of his children are in medical science -- Hannah, a senior specialist in oncology; Mary, a senior specialist in periodontology; and Ruth, a specialist in OBGYN: They are part of the hydrogen peroxide research team.
Thomas E. Levy, M.D., J.D. Board Certified Cardiologist and author. Among his many books is Rapid Virus Recovery, a book on hydrogen peroxide with over 600 scientific citations. [3] He is an inductee of the Orthomolecular Medicine Hall of Fame. [10]
References
- Amoah AGB, Sagoe KW, Quakyi IA, Ayettey-Anie HNG, Ayettey-Adamafio MNB, Ayettey Brew RNA, Newman-Nartey M, Nartey NO, Brightson KTC, Kessie G, Ayettey AS, Konotey-Ahulu FID. (2022) Further observations on hydrogen peroxide antisepsis and COVID-19 cases among healthcare workers and inpatients. J Hosp Infect. 126:103-108. https://pubmed.ncbi.nlm.nih.gov/35594985
- Armogida M, Nisticò R, Mercuri NB. (2012) Therapeutic potential of targeting hydrogen peroxide metabolism in the treatment of brain ischaemia. Br J Pharmacol. 166:1211-1224. https://pubmed.ncbi.nlm.nih.gov/22352897
- Levy TE (2021) Rapid Virus Recovery: No need to live in fear. MedFox Pub. ISBN-13: 9780998312415 https://www.medfoxpub.com/medicalnews/product/RVR/Rapid-Virus-Recovery-No-need-to-live-in-fear
- Caruso AA, Del Prete A, Lazzarino AI (2020) Hydrogen peroxide and viral infections: A literature review with research hypothesis definition in relation to the current covid-19 pandemic. Med Hypotheses 144:109910. https://pubmed.ncbi.nlm.nih.gov/32505069
- Levy TE (2020) COVID-19: How can I cure thee? Let me count the ways. Orthomolecular Medicine News Service. http://orthomolecular.org/resources/omns/v16n37.shtml
- Levy TE (2020) Curing Viruses with Hydrogen Peroxide: Can a simple therapy stop the pandemic? Orthomolecular Medicine News Service. http://orthomolecular.org/resources/omns/v16n43.shtml
- Levy TE (2021) Hydrogen Peroxide Nebulization and COVID Resolution: Impressive anecdotal results. Orthomolecular Medicine News Service. http://orthomolecular.org/resources/omns/v17n13.shtml
- Cheng RZ (2020) Protected Population Immunity, not a Vaccine, is the Way to Stop Covid-19 Pandemic. J Clin Immunol Immunother 6:1-4.
- Profile of Richard Cheng. https://isom.ca/profile/richard-cheng
- Profile of Thomas Levy. https://isom.ca/profile/thomas-levy
Nutritional Medicine is Orthomolecular Medicine
Orthomolecular medicine uses safe, effective nutritional therapy to fight illness. For more information: http://www.orthomolecular.org
Find a Doctor
To locate an orthomolecular physician near you: http://orthomolecular.org/resources/omns/v06n09.shtml
The peer-reviewed Orthomolecular Medicine News Service is a non-profit and non-commercial informational resource.
Editorial Review Board:
Albert G. B. Amoa, MB.Ch.B, Ph.D. (Ghana)
Seth Ayettey, M.B., Ch.B., Ph.D. (Ghana)
Ilyès Baghli, M.D. (Algeria)
Ian Brighthope, MBBS, FACNEM (Australia)
Gilbert Henri Crussol, D.M.D. (Spain)
Carolyn Dean, M.D., N.D. (USA)
Ian Dettman, Ph.D. (Australia)
Susan R. Downs, M.D., M.P.H. (USA)
Ron Ehrlich, B.D.S. (Australia)
Hugo Galindo, M.D. (Colombia)
Martin P. Gallagher, M.D., D.C. (USA)
Michael J. Gonzalez, N.M.D., D.Sc., Ph.D. (Puerto Rico)
William B. Grant, Ph.D. (USA)
Claus Hancke, MD, FACAM (Denmark)
Tonya S. Heyman, M.D. (USA)
Patrick Holford, BSc (United Kingdom)
Suzanne Humphries, M.D. (USA)
Ron Hunninghake, M.D. (USA)
Bo H. Jonsson, M.D., Ph.D. (Sweden)
Dwight Kalita, Ph.D. (USA)
Felix I. D. Konotey-Ahulu, MD, FRCP, DTMH (Ghana)
Jeffrey J. Kotulski, D.O. (USA)
Peter H. Lauda, M.D. (Austria)
Alan Lien, Ph.D. (Taiwan)
Homer Lim, M.D. (Philippines)
Stuart Lindsey, Pharm.D. (USA)
Pedro Gonzalez Lombana, MD, MsC, PhD (Colombia)
Victor A. Marcial-Vega, M.D. (Puerto Rico)
Juan Manuel Martinez, M.D. (Colombia)
Mignonne Mary, M.D. (USA)
Jun Matsuyama, M.D., Ph.D. (Japan)
Joseph Mercola, D.O. (USA)
Jorge R. Miranda-Massari, Pharm.D. (Puerto Rico)
Karin Munsterhjelm-Ahumada, M.D. (Finland)
Tahar Naili, M.D. (Algeria)
W. Todd Penberthy, Ph.D. (USA)
Zhiyong Peng, M.D. (China)
Isabella Akyinbah Quakyi, Ph.D. (Ghana)
Selvam Rengasamy, MBBS, FRCOG (Malaysia)
Jeffrey A. Ruterbusch, D.O. (USA)
Gert E. Schuitemaker, Ph.D. (Netherlands)
Han Ping Shi, M.D., Ph.D. (China)
T.E. Gabriel Stewart, M.B.B.CH. (Ireland)
Thomas L. Taxman, M.D. (USA)
Jagan Nathan Vamanan, M.D. (India)
Garry Vickar, M.D. (USA)
Ken Walker, M.D. (Canada)
Anne Zauderer, D.C. (USA)
Andrew W. Saul, Ph.D. (USA), Editor-In-Chief
Associate Editor: Robert G. Smith, Ph.D. (USA)
Editor, Japanese Edition: Atsuo Yanagisawa, M.D., Ph.D. (Japan)
Editor, Chinese Edition: Richard Cheng, M.D., Ph.D. (USA)
Editor, French Edition: Vladimir Arianoff, M.D. (Belgium)
Editor, Norwegian Edition: Dag Viljen Poleszynski, Ph.D. (Norway)
Editor, Arabic Edition: Moustafa Kamel, R.Ph, P.G.C.M (Egypt)
Editor, Korean Edition: Hyoungjoo Shin, M.D. (South Korea)
Editor, Spanish Edition: Sonia Rita Rial, PhD (Argentina)
Contributing Editor: Thomas E. Levy, M.D., J.D. (USA)
Contributing Editor: Damien Downing, M.B.B.S., M.R.S.B. (United Kingdom)
Assistant Editor: Helen Saul Case, M.S. (USA)
Technology Editor: Michael S. Stewart, B.Sc.C.S. (USA)
Associate Technology Editor: Robert C. Kennedy, M.S. (USA)
Legal Consultant: Jason M. Saul, JD (USA)
Comments and media contact: drsaul@doctoryourself.com OMNS welcomes but is unable to respond to individual reader emails. Reader comments become the property of OMNS and may or may not be used for publication.
Acknowledgement Citation
Click here to see a web copy of this news release: https://orthomolecular.acemlna.com/p_v.php?l=1&c=242&m=241&s=c7ae1002d2f579a22c16a1b89c854212
Comments:
-
No Article Comments available