Positive Health Online
Your Country
Bruxism, TMJD and Migraines - The Terrible Triad
by Dr Yasmin Shakarchy(more info)
listed in dentistry, originally published in issue 255 - June 2019
Definitions
- Bruxism: According to an international panel of experts, the definition of bruxism is “a repetitive jaw-muscle activity characterized by clenching or grinding of the teeth and/or by bracing or thrusting of the mandible.”[1]
- TMJD (or TMD): Temporomandibular joint dysfunction is described as “a clinical term referring to musculoskeletal disorders affecting the temporomandibular joints and their associated musculature.” Often TMJD is synonymous with TMD ( temporomandibular disorders.)[2]
- Migraines: The international Headache society defines chronic migraines as the occurrence of headaches on 15 days or more per month for at least 3 months. These attacks must fulfil the criteria of symptoms without aura on at least 8 days per month for at least 3 months. There must be no use of medication or any other causative factors.[3]
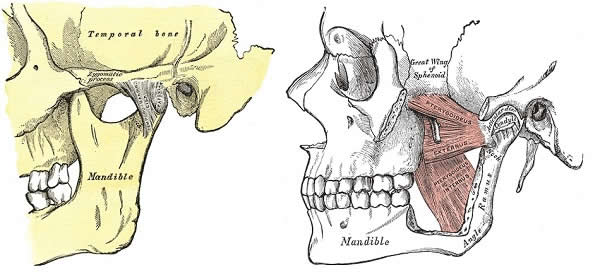
Temporomandibular Joint (left) and The left medial pterygoid muscle (right),
involved in TMJD and Bruxism
Background
Each of the above is a condition in its own right, but as we explore the symptoms, pathophysiology and occurrence, we find that they are very closely linked. This article looks to explore the association and connection between these three areas.
The temporomandibular joint (TMJ) is the hinge that connects the lower jawbone (mandible) to the rest of the skull. This joint is connected to different parts of the body including the face, cheeks, neck and shoulders through various different muscles. When issues arise with the TMJ it may be as a result of joint misalignment, incorrect positioning of teeth or a misaligned bite.[2]
However in most cases TMJD is due to bruxism (teeth grinding) particularly at nighttime. This can result in excessive strain on the associated muscles. If the muscles of the head and face are affected, this can lead to migraine attacks. Other symptoms of TMJD include: Jaw locking and popping, restricted jaw movement, neck and shoulder pain and pain while chewing.[4]
Epidemiology
Bruxism
It can be difficult to find accurate data regarding the prevalence of bruxism. This is largely due to the way it is defined and the way data is collected. Often studies use self-reported bruxism which can be inaccurate as most people are not aware they have this parafunctional habit.[6]
The international classification of sleep disorders (ICSD-R) states that 85–90% of the general population grind their teeth to a degree at some point during their life, however only 5% will develop a clinical condition. Some studies have reported that awake bruxism affects females more commonly than males, while in sleep bruxism, males and females are affected equally.[6]
Migraines
It is estimated that there are 190,000 migraine attacks experienced every day in the UK. 6 million people suffer from migraines in the UK. The prevalence tends to be higher in women than men, with 5-25% of women reporting they suffer with migraines, compared with 2-10% of men.[3, 7]
TMJD
The prevalence of temporomandibular joint dysfunction (TMJD) is between 5% and 12%. What is quite unusual for a chronic pain condition, in that sufferers tend be of a younger age group.[2] The prevalence of TMJD in the headache population is 56.1%.[5]
Pathophysiology
TMJ pain is significantly more frequent in headache patients.[5] The cause and effect relationship between them is still being debated with it being suggested that there is a common pathogenesis. While some studies show that chronic headache patients are more prone to TMJ and masticatory muscle pain (suggesting these headaches are a risk factor for TMJD) other studies show the contrary, in that TMJD may stimulate the occurrence of headaches.[8].
The trigeminal nerve supplies the muscles of mastication around the temporomandibular joint. The neurons in the trigeminal system integrate nociceptive input from TMJ and masticatory muscles. Studies have reported that because of the overlap of innervations with the trigeminal nerve, TMJD therefore causes headaches or is at least a perpetuating factor for migraines as it acts as a constant input increasing the sensitization to pain.[8] With bruxism, which is commonly nocturnal in nature, patients are essentially clenching and grinding their teeth for most of the time while they are sleeping. This then leads to TMJD and migraine attacks.
Diagnosis
Most people don’t realize that their TMJ could be the cause of their migraines, and so misdiagnosis and incorrect treatment provision is usually the case. Pioneering research has solidified this link between chronic migraines and a temporomandibular disorder, with findings showing that the presence of TMJD increases the severity and frequency of migraine attacks.
The relationship between TMJD, bruxing and migraines has been demonstrated in many studies. Furthermore, there is a strong link between bruxism and anxiety/emotional state. Those who have higher levels of stress and anxiety throughout the day, often clench or grind their teeth more frequently in the night.[9] Emotional stress and anxiety disorders were recognized as important factors among bruxing adults. The symptoms of TMJD are very similar to tension, sinus and cluster headaches and so differentiating between these to reach a definitive diagnosis can be difficult.[10]
If TMJD is suspected through bruxing or patients are experiencing chronic repeated episodes of migraine attacks, it is key to see a doctor or dentist. The dentist may be more ideally placed to provisionally diagnose TMJD, and refer you on to an oral and maxillofacial specialist for further assessment and a definitive diagnosis.
The specialist will assess accordingly through taking a detailed history of the symptoms and carrying out full extra-oral as well as intra-oral examinations. The jaw is assessed and checked for clicking sounds at the joint, range of jaw motion as well as palpating the surrounding muscles for any tenderness. Further investigations may be carried out through x-rays, CT scans and even MRI to provide detailed images of the bones involved in the joint, along with the joint’s disk and surrounding soft tissue. This will aid in establishing a definitive diagnosis.
Treatment Options
TMJD and chronic migraines can affect patients’ quality of life significantly. Knowing what treatment options are available is crucial for sufferers.[11]
- Medication
Analgesics particularly anti-inflammatory medication such as Ibuprofen may ease the symptoms of TMJD, however in most cases may not be strong enough. Often clinicians will prescribe Tricyclic antidepressants such as Amitriptyline. These medications are used mostly for depression, but in low doses, they can be prescribed for pain relief, bruxism control and sleeplessness. [12]
Another group of medicines which may help relieve the pain are muscle relaxants such as Diazepam. These types of drugs are sometimes used for a few days or weeks to help relieve pain caused by TMJ disorders created by muscle spasms.[12] - Non-Medication treatment
Occlusal splints or mouth guards are fabricated for patients who are bruxing. The appliance is worn over the lower or upper teeth, and is made from either a soft or hard acrylic, with various thicknesses. The idea is that neuromuscular harmony is achieved in the masticatory system by creating a mechanical disadvantage for these bruxing parafunctional forces. A properly constructed splint ensures a mutually protected bite, whereby the forces created through this habit are minimal. This then aids in muscle relaxtion and repositioning of the TMJ.[13, 14] - Physiotherapy
Along with jaw exercises to stretch and strengthen jaw muscles, other treatments can include using alternating hot and cold compress on the joint and muscles to alleviate pain. As well as sticking to a soft diet to prevent further over-working of the joint and muscles.[15] - Counselling and Therapy
Education and counseling can help patients understand the factors and behaviors that may aggravate the jaw pain or migraine attacks. Furthermore, through counselling and behavioural therapy, stress and anxiety levels may be lowered which in turn may reduce the amount and severity of bruxism in turn aiding to reduce symptoms of TMJD and migraine attacks. [14,16] - Surgery
For patients who do not respond to the above non-surgical treatments, there may be a need for surgical intervention.
Arthroscopy and Arthocentesis
If damage to the TMJ and disc is severe, an arthroscope is used to look inside and assess the temporomandibular joint. Often the surgeon will wash out the joint and perform surgical procedures such as smoothing the bone or repositioning the disc if required. Recent studies have shown that the repeated process of arthocentesis compared with a single procedure, produces a more significant treatment outcome.[17, 18] - Injections
Steroid Injections.
In some people, corticosteroid injections into the joint may be helpful to alleviate pain in the TMJ and restricted mouth opening. This can be done in conjunction with the above surgery.[12, 19]
Botulinum toxin type A (BOTOX)
Botulinum toxin commonly known as BOTOX®, it is a muscle relaxant which in the case of TMJD and migraines, is injected into the temporalis and masseter face and jaw muscles.[20] BOTOX relieves jaw tension by making these muscles unable to engage in the act of bruxing. This alleviates the symptoms of TMJD and migraines It is actually the long-term treatment with BOTOX being delivered at consistent intervals of 4-6 months that produces the best results in alleviating patient symptoms.[11, 12, 21]
Conclusion
The pain and symptoms associate with TMJD and Migraines can severely impact ones quality of life. The link and association between Bruxism, TMJD and Chronic migraines is prevalent in the literature, and many studies have aimed to understand the biology and physiological connection between these. Although more research is needed in this area, we know that appropriate diagnosis is key for successful management and ultimately alleviating the debilitating symptoms associated.
References
1. Sriharsha P, Gujjari AK, Dhakshaini MR, Prashant A. Comparative Evaluation of Salivary Cortisol Levels in Bruxism Patients Before and After Using Soft Occlusal Splint: An in vivo Study. Contemp Clin Dent 9(2):182-187. Apr-Jun 2018.
2. U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES: National Institutes of Health Publication No. 17-3487 (September 2017) TMJ Disorders, Available at: https://www.nidcr.nih.gov/sites/default/files/2017-12/tmj-disorders.pdf [Accessed 01 March 2019].
3 . National Institute for Health and Care Excellence (August 2011) Final scope for the appraisal of botulinum toxin type A for the prophylaxis of headaches in adults with chronic migraine. Available at: https://www.nice.org.uk/guidance/TA260/documents/migraine-chronic-botulinum-toxin-type-a-final-scope2 [Accessed 01 March 2019].
4. Stuginski-Barbosa J, Macedo HR, Bigal ME, Speciali JG. Signs of temporomandibular disorders in migraine patients: a prospective, controlled study. Clin J Pain 26(5):418-21. Jun 2010.
5. Ballegaard V Thede-Schmidt-Hansen P, Svensson P, Jensen R. Are headache and temporomandibular disorders related? A blinded study. Cephalalgia 28(8): 832-41. Aug 2008.
6. Thorpy MJ. Classification of Sleep Disorders. Neurotherapeutics 9(4): 687–701. October 2012.
7. Johansson A, et al. Gender difference in symptoms related to temporomandibular disorders in a population of 50-year-old subjects. J OROFAC PAIN17: 29-35. 2003
8. Zenkevich AS, Filatova EG, Latysheva NV. Migraine and temporomandibular joint dysfunction: mechanisms of comorbidity. Zhurnal Nevrologii i Psikhiatrii Imeni S.S. Korsakova 115(10): 33-38. Jan 2015.
9. Yavuz GE, Aytemiz C. Investigation of relation between anxiety and TMJ dysfunction in dental students. Ankara Univ Hekim Fak Derg 16(3): 439-46. September 1989.
10. Kuhn M, Türp JC. Risk factors for bruxism. Swiss Dent J 128(2): 118-124. February 2018.
11. Villa S, Raoul G, Machuron F, Ferri J, Nicot R. Improvement in quality of life after botulinum toxin injection for temporomandibular disorder. J Stomatol Oral Maxillofac Surg 120(1): 2-6. February 2019.
12. Ouanounou A, Goldberg M, Haas DA. Pharmacotherapy in Temporomandibular Disorders: A Review. J Can Dent Assoc 83:h7. 2017.
13. Hamda T, Kotani H, Kawazow Y, Yamada S. Effect of occlusal splints on the EMG activity of masseter and temporal muscles in bruxism with clinical symptoms. J Oral Rehabil 9(2): 119-23. March 1982.
14. Giannakopoulos NN, Katsikogianni EN, Hellmann D, Eberhard L, Leckel M, Schindler HJ, Schmitter M. Comparison of three different options for immediate treatment of painful temporomandibular disorders: a randomized, controlled pilot trial. Acta Odontol Scand 74(6): 480-6. August 2016
15. Häggman-Henrikson B, Wiesinger B, Wänman A. The effect of supervised exercise on localized TMD pain and TMD pain associated with generalized pain. Acta Odontol Scand 76(1) 6-12. January 2018.
16. Costa YM, Porporatti AL, Stuginski-Barbosa J, Bonjardim LR, Speciali JG, Rodrigues Conti PC. Headache Attributed to Masticatory Myofascial Pain: Clinical Features and Management Outcomes. J Oral Facial Pain Headache 29(4): 323-30. 2015.
17 . Kütük N, Baş B, Kazan D, Yüceer E. Is Repeated Arthrocentesis Beneficial in the Treatment of Temporomandibular Disorders: A Retrospective Study. J Oral Maxillofac Surg 5. February 2019
18. Ohnishi M. Arthroscopy and arthroscopic surgery of the temporomandibular joint (T.M.J.). Rev Stomatol Chir Maxillofac 91(2): 143-50. 1990.
19. Samiee A, Sabzerou D, Edalatpajouh F, Clark G, Ram S. Temporomandibular joint injection with corticosteroid and local anesthetic for limited mouth opening. Journal of Oral Science 53(3): 321-5. September 2011.
20. Connelly ST, Myung J, Gupta R, Tartaglia GM, Gizdulich A, Yang J, Silva R. Clinical outcomes of Botox injections for chronic temporomandibular disorders: do we understand how Botox works on muscle, pain, and the brain? Int J Oral Maxillofac Surg. 46(3): 322-327. March 2017.
21. Vikelis M, Argyriou AA, Dermitzakis EV, Spingos KC, Makris N, Kararizou E. Sustained onabotulinumtoxinA therapeutic benefits in patients with chronic migraine over 3 years of treatment. J Headache Pain 19(1): 87. September 2018.
Comments:
-
No Article Comments available