Positive Health Online
Your Country

Interdisciplinary Bodywork for Best Results
by Leon Chaitow, ND DO(more info)
listed in bodywork, originally published in issue 59 - December 2000
Despite being pretty well informed as to manipulative methods in general, and soft tissue manipulation in particular, I had not come across this term (which stands for sustained neutral apophyseal glides). The method was duly explained and demonstrated and I was impressed by its simplicity, elegance and ease of use. This gentle and effective method certainly has echoes of osteopathic PRT methodology, but with unique characteristics.
I have since learned the basics of SNAGS (and its cousin NAGS as well as other 'mobilization with movement' – MWM methods – all devised by Mulligan). As a result of combining this excellent physical therapy modality with my usual osteopathic approaches, my patients have benefited, and I have to work less hard to achieve results when dealing with particular problems.
My gripe is, 'Why didn't I know about SNAGS earlier?'
Cross-fertilization of this sort ought to be happening all the time, as the best of all the different bodywork systems are exchanged, compared, refined and used by ALL. But are they? When I mentioned my SNAGS experience to a group of osteopaths at a postgraduate lecture, none had heard of it. Likewise, when I was working with massage therapists and chiropractors, an almost total lack of awareness of this method was apparent.
Another idea that has emerged out of physiotherapy is proprioceptive taping.
In one version of osteopathic PRT, known as functional technique, osteopaths carefully palpate, guide and ease dysfunctional tissues, joints, or areas (especially acutely irritated or painful ones) into their positions of 'maximum ease'. The tissues are then usually held in this ease state for several minutes, in order to allow irritated neural structures to modulate their firing patterns, as well as for circulatory enhancement to occur in what were previously tense, restricted, probably ischaemic and often painful structures.
It emerges that, independently of these osteopathic methods (PRT), which have been around since the 1950s, physiotherapy has evolved methods which, rather than manually holding tissues in their 'ease' position, actually tapes them into a comfortable, 'unloaded', state and leave them this way overnight, or even for several days at a time.
How obvious, how logical, how simple and how strange that osteopaths did not think of this concept of what could be called 'sustained PRT'.
But then neither did physiotherapists think of simply holding acutely strained tissues in 'ease', for just a few minutes, in order to produce a beneficial change!
It is certainly possible to continue developing a list which compares new and traditional ways of treating tissues, and to elaborate on the different and yet similar solutions various professions have found for treating similar problems (after all they are all working on identical human problems!). But I believe I have made the points necessary to continue with the theme of this article – that everyone would benefit (therapist and patient) if each of the distinctive bodywork professions would drop their defensive guards and actively examine and learn from professions they usually view with suspicion, as rivals.
Reflecting on what works best in treating musculoskeletal pain and dysfunction, it has become clear to me that the wider the selection of therapeutic techniques and methods a practitioner/ therapist has available, the greater the chance of being able to appropriately address the needs of the patient, and of the multiple dysfunctional conditions which present for care.
This may seem to be stating the obvious, and is anything but an earth-shattering observation. However, its very simplicity makes the fact that it is not more widely applied something of a mystery to me.
For example (note that this is a selection, not a comprehensive list):
• Why do so many massage therapists remain locked into using only traditional techniques which, while extremely useful, are limited in their value (and far more energy- and time consuming) in addressing chronic soft tissue and joint problems, as well as often being contraindicated in extremely acute situations – especially because a range of soft tissue methods deriving from other professions, which fit well with what they already do, are now so widely taught? In fact, why do most massage training establishments fail to incorporate the best of osteopathic soft tissue methodology, for example?
• Why do osteopaths not use more chiropractic methods, and vice versa (although, to be fair, cross-fertilization between these professions is slowly becoming more widespread)?
• Why don't all physiotherapists learn osteopathic and chiropractic manipulative methods, instead of just those few who belong to manipulative therapy special interest groups?
• Why do the majority of osteopaths and chiropractors not have training in the postural, breathing and general use, rehabilitation skills, which are basic to physiotherapists (although special interest
courses in rehabilitation and prevention methods are very slowly evolving in both chiropractic and osteopathy)?
• Why don't all bodywork practitioners and therapist learn the basics of Feldenkrais, Alexander and/or Pilates methods, so that they can better re-educate their patients as to how to use themselves safely?
• And why do doctors (GPs especially) not learn basic palpation skills and simple first aid measures using, for example, muscle energy technique (MET) or PRT? In postgraduate modules it is possible to teach such methods, in just a few hours, to people with a reasonable knowledge of anatomy and physiology. These methods are also suitable to be taught to patients for self-care, something nurses and GPs should be able to do!
It is clear that by crossing interdisciplinary boundaries, many of which are quite artificial, and which are commonly more politically than professionally valid, it is possible to acquire skills that are often only taught within the framework of particular professions. And it should only be a small step from professionals learning from each other in postgraduate settings, to the professional training courses incorporating the methods of other professions into their curricula. A good example of this is seen in the rapidity with which the physiotherapy profession adopted acupuncture as a basic part of its training, rather than leaving it to postgraduate courses, as other professions have done. The natural end result of such a process, which I predict will become inevitable over the next 50 years or so as rationalization and evidence-based methodology become the norm, will be a merging of the professions of osteopathy, chiropractic and modern physiotherapy. By that time the professions adjunctive to these complete systems, such as PT-assistant, or chiropractic assistant, and quite possibly of massage therapist, will also have merged.
In that most advanced of countries, which so easily sheds traditional, stultifying approaches, Australia, there is already training of both osteopathy and chiropractic within the same teaching establishments (for example the Royal Melbourne Institute of Technology), with students of the two disciplines sharing core subjects.
Another factor worth considering in this evolution towards the harmonization of professions is the development of e-learning. Already under active development in the USA are home-learning courses (to BSc level) in (for example) massage therapy, which will, as a matter of course, incorporate many of the methods I have mentioned above, as integral aspects of the curriculum. These distance-learning approaches will be coupled with intensive residential periods of instruction and evaluation, and will create a basis for a wide range of bodywork skills to be acquired from the home computer, using interactive programmes including dissection on screen!
Personal Experience
Let me try to explain how these thoughts relate to my own professional and personal experiences, and why I categorically know how important cross-fertilization is in enlarging the potential of practitioners as well as in ensuring optimal benefit for patients.
I trained as an osteopath and a naturopath, graduating in 1960. Osteopathy as I learned it, comprised a variety of manipulative techniques which can loosely be categorized as involving either high velocity thrust (HVT), or articulation/ mobilization techniques, associated with some fairly unrefined general soft tissue approaches, based on basic massage strokes (effleurage, etc).
Fortunately, enough my early years of practice involved working for, and with, one of the pioneers of neuromuscular technique (NMT), my late uncle Boris Chaitow ND, DC, DO. For the first year of this virtual apprenticeship (despite, after four years of training, being a graduate DO!), the only work he allowed me to do was to observe him working (and NMT formed the basis of all his manual approaches so I saw a great deal of this) as well as answering the phone and making appointments. I was then, for another year, allowed to perform NMT (with very little additional manipulation) on those of his patients he was willing to sacrifice to my tentative ministrations. In this way, NMT became the basis of my future work, with active manipulation (HVT especially) slowly falling into the background, to be used only when soft tissue methods failed to restore normal function to restricted joints (and soft tissue approaches work 8 times out of 10, in my experience).
NMT has proved to be an extremely useful soft tissue manipulation method (which incidentally derived in the 1930s in large part from the work of an Ayurvedic practitioner Dr Varma). NMT may be used for assessing dysfunctional tissue states in general, or for localizing discrete 'points' that act as triggers to wider dysfunction. In addition, NMT is used for preparing joints for subsequent manipulation, or for the normalization of restricted, fibrotic or otherwise dysfunctional soft tissues, including the deactivation of myofascial trigger points.
In various postgraduate courses and classes over the past 35 to 40 years, I have also acquired a reasonable working knowledge of orthomolecular nutrition, acupuncture, cranial osteopathy, osteopathic muscle energy and positional release techniques (MET, PRT), and am increasingly incorporating myofascial release (MFR) methodology, in one form or another, as well as MWM (SNAGS). In addition, I had a relatively brief (but meaningful) introduction to a form of psychotherapy known as voice dialogue.
Do I really need to have this variety of tools available? Absolutely, and I suggest so do all manual therapists. I also feel the lack of several important methods which I have not (as yet – I am after all only 62) had time to master, including manual lymph drainage (MLD) and Feldenkrais methodology.

Neuromuscular Technique (NMT) – Operator's posture should ensure a straight treating arm for ease of transmission
of body weight, as well as leg positions which allow for the easy transfer of weight and the centre of gravity.
These postures assist in reducing energy expenditure and ease spinal stress.

First stage of Integrated Neuromuscular Inhibition Technique (INIT) in which a tender/pain/trigger point in
supraspinatus is located and ischaemically compressed, either intermittently or persistently
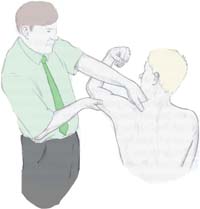
The pain is removed from the tender/pain/trigger point by finding a position of ease which is held for at least 20 seconds,
following which an isometric contraction is achieved involving the tissues which house the tender/pain/trigger point

Following the holding of the isometric contraction for an appropriate period, the muscle housing the point
of local soft tissue dysfunction is stretched. This completes the INIT sequence
Case Studies
Let me offer a few examples that highlight the need for 'bodyworkers' of all denominations to acquire skills from other professions. Note that these case studies are based on real patients, but they have been suitably camouflaged to protect confidentiality.
Case Study 1 – Mary
Mary, aged 28, consulted me two weeks following a motor accident in which she had acquired a severe whiplash injury to the neck. Mary's symptoms ranged from radiating neck and arm pain, to chronic (almost constant) headache and virtually incapacitating dizziness and imbalance. Research suggests that damage such as tearing of the end plates of discs, and to facet joints, is responsible for many of the symptoms following whiplash.[1] Mary appeared to meet the Quebec task force classification of Category lll (neck complaint with neurological signs)[2] – with common whiplash symptoms ranging from radiating neck and arm pain, to chronic headache and virtually incapacitating dizziness and imbalance. Whiplash-associated disorders have attracted a wide range of (apparently mostly useless) treatment strategies. For example, unfortunately Mary had been put in a collar at the emergency hospital room, and had been wearing it constantly for two weeks. Thankfully I was aware that this was undesirable.
"Collars are probably contraindicated for whiplash…they irritate jaws, foster joint adhesions, and lead to tissue atrophy."[3] I was, however, also aware that research showed that short term manipulation and mobilization can be helpful.[3]
Weekly treatment record:
First session: positional release technique (PRT) only, consisting of functional and strain/counterstrain methods), plus advice on removal of the collar and home treatment with ice, rest and basic PRT self-treatment.[4]
Second session: by this time symptoms were approximately 30% improved (based on self-assessment visual analog scale) but with headache and dizziness unchanged; NMT and MET to release hypertonicity in upper thoracic and cervical muscles (particularly levator scapula, upper trapezius, scalenes and sternocleidomastoid) plus PRT to ease extreme sensitivity in the short extensors of the head. Home treatment involving careful positional release self-applied, was explained and demonstrated for daily use.
Third session: by this time symptoms were reduced to 40% of original levels, still involving severe headache, dizziness and some intermittent shoulder/arm pain; NMT, MET and PRT were applied to the soft tissues, followed by a positional release of the 1st rib which was elevated, as well as application of Mulligan's SNAGS method to release facet joint restriction at C6 and 7 levels.[5,6] This latter approach produced almost instant relief of head symptoms, ostensibly as a result of freeing the blocked facet joints.
4th session (six weeks post trauma): residual symptoms of mild stiffness on waking were all that was reported. All shoulder/arm problems as well as the headache and dizziness had vanished within two days of the previous treatment. General NMT was performed, a cranial 'fascial balancing' treatment was performed, and advice given on long-term postural strategies with a recommendation to see an Alexander or a Feldenkrais teacher.
Follow-up after 3 months: spent discussing general health-enhancing strategies. There were no residual neck problems or symptoms. Mary was seeing a certified Feldenkrais practitioner for a course designed to assist her to use her body more efficiently.
Based on having treated similar problems for many years, I am as certain as I can be that the excellent results obtained with Mary would not have been possible, and certainly not as rapidly, without the array of techniques employed.
We need to have a full toolbox, and select from this appropriately!
Case Study 2: David
David, aged 40, consulted me with fatigue and general muscular pain. He had seen a neurologist who diagnosed chronic fatigue syndrome, although his own doctor considered that the condition might be fibromyalgia. His case history was complex and space does not permit a full recounting of it here. Suffice to say that the aspect of David's condition that attracted my initial interest was his appalling breathing pattern, which involved shallow upper chest activity interspersed with gasps and sighs as 'air hunger' manifested. His history included periods of extreme anxiety and panic attacks, culminating in phobic behaviour. This had been treated medically (drugs) and by cognitive behaviour modification. His fatigue and muscular pain problems had emerged slowly over the years, but had become more severe following his treatment with anxiolytic drugs. Significantly, no one had ever approached the problem from the perspective of trying to help David to normalize his breathing.
At the first consultation a detailed nutritional evaluation was made, which together with his symptoms and evidence from manual palpation, led to specific suggestions being made:
All caffeine and alcohol were to be avoided (David drank both moderately) as they negatively influenced all his symptoms.[7] David's sugar intake was cut drastically for similar reasons.[8]
Calcium and magnesium were prescribed (1000mg/500mg daily) as he demonstrated a positive Chvostek sign (a sign of latent tetany, which probably involves calcium and or magnesium deficiency is evident when a small reflex hammer is used to tap the soft part of the cheek, avoiding the zygomatic arch). If a lightning-like contraction occurs the test is positive.[9]
Basic instruction was given in the use of 'anti-arousal' breathing which is based on pranayama yoga, and which has been researched to show a calming effect on anxious individuals.[10]
Bodywork sessions were scheduled to attempt to release his tense and tight respiratory apparatus: thoracic spine, ribs, intercostals, diaphragm, accessory breathing muscles – as well as to deactivate a number of active trigger points I had identified by palpation in his upper abdominal, intercostal, pectoral, scalene and upper trapezius muscles.
Over the following six weeks, David was seen weekly, after which fortnightly sessions were arranged. During this time a combination of NMT, PRT and MET was used to achieve a gradual improvement in the structures identified as dysfunctional and to deactivate the trigger points.
The method used to deactivate trigger points involves a sequence of using NMT, PRT and MET, called integrated neuromuscular inhibition technique (INIT) which incorporates and integrates sequentially a number of different methods, for optimal results in effectively eliminating the reflexive behaviour of myofascial trigger points.[11]
Treatment, as described, has thus far (after six months) resulted in a marked improvement in David's symptoms – with visual analog pain scores of around 4 to 5, compared with 9 or 10 at the outset. His fatigue levels have improved at approximately the same rate, although there are periodic setbacks, possibly related to environmental or food sensitivities/allergies thus far not identified.
Treatment now continues at monthly intervals, with an associate when I am abroad, and with me when I am in London.
My prognosis, based on past experience of similar cases, suggests that David will require regular attention (bodywork and nutritional guidance) at roughly this level for another six months or so, after which, if progress is maintained, a periodic check-up to ensure his improvement is maintained – say every six months – would be advisable.
In this example a combination of bodywork approaches together with rehabilitation strategies (breathing in particular) can be seen, in association with nutritional modification, to have changed a situation verging on dysfunctional, to a pattern of reasonable functionality. Had I had more of a training in psychotherapy I have no doubt some of the deeper causes of David's anxiety may have been addressed, and this remains an area in which I feel deficient. Since David resists all suggestions to see a counsellor or psychotherapist, my own primitive efforts in this direction have to suffice.
Conclusion
Hopefully these two examples give a clear message: We cannot depend on single therapeutic interventions when faced with complex conditions and situations. We need to be able to choose methods which are more appropriate in acute or in chronic situations, and which complement each other. We must learn from each other and begin the inevitable process of the merging of methods and ultimately of professions. Therapists with the least formal training can upgrade their skills base enormously by ensuring proficiency in methods such as NMT, PRT, MET, MFR etc., as well as educational approaches such as those exemplified by Alexander technique and Feldenkrais, as long as these are built onto a solid foundation of anatomy, physiology and pathophysiology.
References
1. Cassidy J. Quebec Task Force on Whiplash Associated Disorders. J Musculoskeletal Pain. 4(4): 5-9. 1996.
2. Spitzer W, Skovrom M and Salmi L. Scientific Monograph of the Quebec Task Force in Whiplash-related Disorders. Spine. 20(8S). 1995.
3. Allen ME (ed.). The New Whiplash, Musculoskeletal Pain Emanating from the Head and Neck. Haworth Medical Press. New York. 1996.
4. Chaitow L. Positional Release Techniques. Churchill Livingstone. Edinburgh. 1996.
5. Chaitow L. Muscle Energy Techniques. Churchill Livingstone. Edinburgh. 1996.
6. Chaitow L. Modern Neuromuscular Techniques Churchill Livingstone. Edinburgh. 1996.
7. Uhde T et al. Caffeine and Behaviour – Relationship to Psychopathology and Underlying Mechanisms. Pharmacology Bulletin 20(3): 426-430. 1984.
8. Rainey J et al. Psychopharmacology Bulletin 20(1): 45-49. 1984.
9. Durlach J. Magnesium and Therapeutics. Magnesium Research 7: 313-328. 1994.
10. Cappo B and Holmes D. Utility of Prolonged Respiratory Exhalation for Reducing Physiological and Psychological Arousal in Non-threatening and Threatening Situations. J Psychosomatic Research 28(4): 265-273. 1984.
11. Chaitow L. Fibromyalgia Syndrome: A Practitioner's Guide to Its Treatment. Churchill Livingstone. Edinburgh. 2000.
Comments:
-
No Article Comments available