Positive Health Online
Your Country

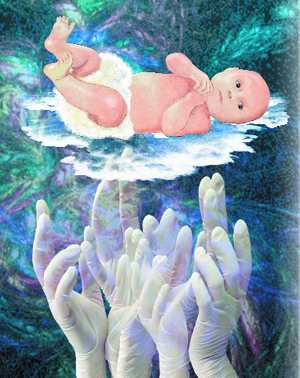
Neonatal Sensitisation to Latex
listed in allergies, originally published in issue 41 - June 1999
Babies born in delivery rooms of hospitals are exposed to latex through skin and mucous membrane contact with pre-powdered latex gloves worn by midwives and doctors, and through the inhalation of latex bound starch powder in the air of the delivery room.
This paper examines the hypothesis that they are at risk for latex sensitisation, and that part of the sharp increase of childhood asthma, eczema and anaphylaxis within the past thirty to forty years may be linked.
These possibilities seem hitherto unsuspected. In over seven hundred papers on latex allergy no mention of neo-natal exposure to latex has been found. Even obstetric papers discussing the risks for an atopic mother (atopic – a tendency to develop allergies) do not seem to anticipate any risk for the baby, who might also be atopic.
Latex allergy is primarily regarded as an occupational hazard. This paper suggests that it is a hazard for every baby handled by latex gloves at birth.
The modern epidemic of allergic diseases is due to many, possibly thousands, of environmental and nutritional allergens. Whilst recognising that there are many other possible causes for infant sensitisation, this paper focuses specifically on latex and chemicals.
Natural latex rubber is derived from hevea brasiliensis. It contains many major and minor components, some of which are powerful allergens.[1] The chemicals used in manufacture, and chemical sterilisers applied to the gloves can also act as contact allergens.[1]
Allergic reactions to latex gloves involve Type I and Type IV hypersensitivity reactions.
Type I – Immediate Reaction
This is an immunological response to allergens which react with immunoglobin E (IgE) antibodies carried on the mast cells and basophils. Symptoms include respiratory distress and asthma, rhinoconjunctivitis, itching of the skin, swelling of the lips, tongue and throat, acute dizziness, abdominal pain, nausea, hypotension, anaphylaxis.[2] Type I reactions occur as an immunological response to latex proteins, through skin contact and the inhalation of latex bound glove powder.[1]
Type IV – Cell Mediated or Delayed Hypersensitivity
Antibodies are not involved, and the reaction depends on activated T-lymphocytes. Symptoms of contact dermatitis result, including redness, swelling, thickening or cracking of the skin, and irritation.[2] Type IV reactions are caused by contact with the chemicals used in glove manufacture and contact with the sterilising agents.[1]
The most commonly observed clinical symptoms of latex allergy are asthma and eczema.
The manufacture of latex rubber gloves
Surgical gloves have been used for most of this century with little ill effects. Manufacture used to be simple, mainly involving boiling the latex at high temperatures. The heat destroyed most of the natural proteins. Gloves were re-used, and were sterilised between uses by boiling or autoclaving. This further destroyed natural proteins. The gloves were supplied with no powder. Surgical gloves used to be made in the UK and European countries.
During the 1970s demand for gloves increased, and manufacture changed. Gloves became cheap, disposable, and pre-powdered. Chemical accelerators were added to the raw latex to speed up the manufacturing process, and sterilisation by means of chemicals was introduced. Patenting laws protected firms from naming these chemicals. It is difficult to discover what chemicals are used as they vary from firm to firm, and are constantly changing. All gloves are now made in Eastern countries.
Modern disposable gloves are pre-powdered and the released powder floats in the air. Latex proteins have been shown to adhere to corn starch glove powder, thus creating a protein-polysaccharide complex which can act as a potent aero-allergen.[3] This will be inhaled by anyone in the vicinity, and can cause acute inflammation of the lungs.[3,4]
Newson and Shaw[5] have made a survey of starch particles and latex proteins in the air of two hospitals. Concentrations of up to 3667 particles per cubic metre were recorded in units where gloves were most frequently used. Rooms with no ventilation showed the highest recordings.
Delivery rooms are small and frequently enclosed, but unfortunately the survey did not include a maternity unit. (Personal communication from Dr S. W. B. Newson.)
Exposure of the new-born to latex
The first hands to touch a new-born baby will be those of a midwife wearing latex rubber gloves. The baby's skin will be handled all over, including sometimes a finger placed in the mouth. The umbilical cord will be handled. It will be clamped and cut. Is it possible for latex allergens to enter the blood stream via the umbilical cord? If pre-powdered latex gloves are used, the air of the delivery room will contain latex bound starch powder; this will be inhaled by the baby with its first breath.
In their early weeks of life, babies should be exposed as little as possible to contact allergens, aero-allergens and chemicals, and for many years there has been evidence linking early exposure with the development of allergic disease.[7]
This paper has been criticised by several immunologists and paediatricians on the grounds that the short period of time during delivery in which a baby is exposed to latex, would not be sufficient to sensitise the baby. They point out that in health workers, large doses of the allergen, over a long period of time, are necessary for latex allergy to develop. But a new born baby is not an adult.
In 1977, E. E. Jarrett in Edinburgh showed, in new-born rats, that IgE sensitisation occurs more easily following the administration of minute doses of parenternal allergen than the administration of a large dose.[7]
These experiments involved cows milk proteins. There have been no similar experiments conducted to assess the level of latex protein required to sensitise a baby. Until such experiments are conducted, and the findings published, no-one can say for certain that a low level of latex exposure at birth would be insufficient to sensitise a baby.
No signs of allergic reaction to latex have been reported in new-born babies. This is because at the time of sensitisation (called the sensitising event) there are no symptoms. Sensitisation is acquired, and it is only on repeated exposure that symptoms develop, starting weeks or years after the initial exposure.
Prematurity
Premature babies and other babies in neo-natal intensive or special care units are at the greatest risk due to longer exposure to the latex allergens from gloves, and inhalation of aero-allergens. In addition latex is used in the equipment of neo-natal intensive care units.
Incubators contain latex. Latex mattresses or rubber sheets are often used. Syringe plungers, vial tops, respiratory face masks, catheters, adhesives, and a great deal of other hospital equipment containing latex will be used, all of which will increase exposure. A premature baby is usually bottle-fed, and the teat may be made of latex.
There is a known link between lung disease and prematurity. In Asthma, Vol. II 1997, it is stated that:
"Prematurity is a major risk factor for wheezing, which is the mildest form of chronic lung disease. Around 50% of very low birth-weight infants develop episodic lower respiratory illness in infancy."[8]
This appears to be a relatively new phenomenon. Neither Conybeare on Asthma (1942)[9] nor Christie Brown on Prematurity (1956)[10] refers to a link between asthma and prematurity. Something must have happened in the care of premature babies during the past forty years to make prematurity a 50% risk factor in the development of lung disease.
According to the National Eczema Society no figures are available about the incidence of eczema in children who were born prematurely. However, the letter pages of the NES journal contain a high proportion of letters about babies with eczema who were also premature babies. This is anecdotal evidence, which deserves further investigation.
Latex sensitisation is irreversible,[7] and sensitised individuals will need to avoid latex altogether. However, this is virtually impossible, because many common household items encountered every day by the baby will include latex. This can be in the cot and pram, the sundry items like sheeting, reins, clothes, toys, rubber bands, elastic. Disposable nappies contain latex, and many health visitors today report chronic dermatitis or nappy rash in babies. Contact of mucosal surfaces with latex is particularly liable to lead to latex allergy.[11] According to the customers' advisory service of Boots the Chemist, all dummies and about 40% of bottle teats are made from latex. The antigens can be absorbed through the oral mucosa. If the mother does not suspect that her baby has been sensitised to latex, and the possibility has not been suggested to her, she will not attempt to provide a latex-free environment for her child. Nor can she be expected to understand cross-reacting allergens.
Cross reactivity
Latex is derived from a plant, and all plants seem to share a common factor which is highly allergenic to some people. At present this factor is unidentified, and there may be more than one.
Two known, specific cross-reactions occur with latex allergy:
1. Food cross-reactions[12-20]
2. Plant and pollen cross-reactions[21]
Food cross-reactions
Latex is very complex and exhibits about 200 distinct polypeptides, which are a major cause of Type I sensitivity. Because the protein allergens of latex are common plant enzymes they may also act as cross reacting proteins in various plant foods.[13] Hevea brasiliensis is related to many tropical and sub tropical fruit trees and the Brehler study of 1997[14] identified fruit specific IgE antibodies in latex sensitive children, confirmed by RAST. Specifically: papaya, mango, avocado, banana, chestnut, passion fruit, fig, melon, kiwi, pineapple, peach, tomato. The Novembre study of 1997[12] identified the same fruit-specific IgE antibodies in latex sensitive children, and found, in addition, sensitivity to apricot, grape, pear, apple, orange and almond.
It is virtually impossible to avoid fruit when weaning a baby and, in any event, this would be undesirable for nutritional reasons. Banana shares many common epitopes with latex.[14] Banana is nearly always given to a baby during weaning. The prevalence of eczema and asthma in children have both increased markedly in the latter half of this century. The National Eczema Society and the British Asthma Campaign both recognise food allergy and intolerance as being a contributory factor in eczema and asthma, but both societies state that the problem is multi-causal and inexplicable. An underlying and unsuspected latex allergy, acquired at birth, might be a partial explanation.
Peanut allergy
Chestnuts and almonds are known to cross react with latex allergy.[12], [14] Children who are allergic to one type of nut are often allergic to other nuts, even though the nuts are not related botanically. Most children with a nut allergy also react to peanuts, even though peanuts are not a tree nut, but a legume.[15]
Peanut allergy is important, because it is a common cause of anaphylaxis, and fatal reactions occur.[16] Its prevalence has increased substantially, with one in two hundred 4 year olds now having this form of allergy.[16, 17] In 1996 Dr Pamela Ewan of Cambridge stated that peanut allergy was known to occur before the age of three in 55% of children with this condition, and during the first year of life in 17%, for which there was no known cause. A study from France found that 8% of babies up to age 4 months had IgE antibodies to peanut allergies.[19] A study from Southampton last year found that 80% of children with peanut allergy reacted to their first known exposure to peanut containing foods.[20] This indicated that they were already sensitised.
In spite of international research and speculation no cause has been found.
I suggest that children who are allergic to peanuts might have been sensitised at birth to latex, and that peanut allergy could be a secondary cross reaction. No research has been conducted in this field.
Pollen and plant cross reactions to latex
Natural latex shares IgE epitopes with certain grasses and weed pollens, specifically mugwort, ragweed, timothy grass, and birch.[21] These are all common plants in temperate zones, and produce a great deal of pollen. In children who react violently to pollen the possibility of a cross reaction to an underlying latex allergy might be considered.
Hevea brasiliensis is a euphorbia. This genus contains over 1000 species, of which more than 100 are native to temperate zones. Most of these plants contain latex, a white juice which oozes from the stem, and which is highly allergenic. Euphorbias are a common cultivated and wild plant, and a child exposed at birth to latex might react on contact with the latex in most of these plants.
No research has been undertaken to suggest that contact dermatitis to euphorbias is related to latex dermatitis, but the possibility deserves examination.
A new classification of plants based on their DNA structure was published in November 1998. The foregoing paragraphs about cross reactivity to the hevea brasiliensis are correct by the new DNA classification. (Personally checked by Dr Mark Chase, head of molecular systematic studies at Jodrell Laboratory, Kew Gardens.)
Chemicals
Part of the problem with environmental chemicals is the process of synergism – the phenomenon in which the combined action of two or more compounds is greater than the sum of the individual effects of each compound. Two chemicals, each of low level, in combination may increase their toxicities ten-fold over each of the chemicals when separate, and three chemicals may increase toxicities one hundred-fold.
The identity, numbers, and combinations of chemicals used in glove manufacture are unknown, and the effects on humans are unknown. It has been estimated that babies may be up to ten times more vulnerable than adults to chemical toxicity.
Allergic reactions to contact with the chemicals used in glove manufacture and the chemical sterilisers used on gloves are well documented.[21] The occupational hazards are widely recognised and warnings to staff are given.[22]
Searches by the Royal College of Midwives and the Royal College of Obstetricians (over two hundred papers) have revealed no literature suggesting that a new-born baby might also react allergically to these chemicals, and no warning that babies should not be touched by these gloves.
Multiple chemical sensitivity is a concept not widely accepted by the medical profession. Nonetheless, pollutants, most of which are chemical, may interact with each other.[23] There is now good evidence of widespread chemical reactions, and this tends to multiply exponentially in sensitised individuals.[24]
Discussion
Until about the 1950s most babies in the UK were born at home. Gloves were expensive and re-used. They were boiled between each use. Many district midwives of my generation can remember that frequently, especially in rural areas, gloves were not worn at all. The drive for safer hospital delivery gained pace, and by the 1970s only 1% of babies were born at home. Hospital midwives deliver 75-80% of all births (Royal College of Midwives Information). Latex gloves are always worn.
In the past 15-20 years the dangers of cheap pre-powdered disposable gloves have been recognised, but although alternatives are available, they are over ten times more expensive. These expensive gloves are generally reserved for doctors. Nurses and midwives usually have to use the cheap ones. In 1992 the Nursing Times reported:[25]
"It is not uncommon to pull from a box glove after glove with holes or tears, or fingers stuck together or missing, before finding two usable gloves."
All the while, latex bound starch powder will be flying into the air of the delivery room where the baby will be born.
Allergists and immunologists, who have little knowledge of the day to day practicalities of midwifery, may be unaware of the degree of exposure for a baby. Midwives and obstetricians who are not trained in allergies, may be unaware of the process of sensitisation, particularly as the baby shows no sign of an allergic reaction in the first few days of life.
Latex allergy in children is considered to be rare, because only a few children show an immediate and obvious hypersensitive reaction to latex. However, low levels of sensitivity may be latent, and not recognised without undergoing special investigative procedure. The child who has asthma, eczema, or a history of anaphylaxis may be tested for common allergens, such as milk or house dust mite, but testing babies or children for latex is rare, because it is unsuspected.
Beyond the special case of children with spina bifida, in whom latex allergy has been reported in up to 70%,[26] there has been very little study of latex allergy in atopic children, and there is no evidence on the means of sensitisation. The Niggerman study of 1998[27] of children with urticaria, eczema, asthma and anaphylaxis, who are latex allergic, states:
"Medical history, certain foods, pacifiers, mattress composition, toys, and socio-economic data proved not to be a significant risk factor in latex sensitisation." (my italics), and concludes:
"Besides the number of operations and the atopic pre-disposition no other defining risk factors for developing sensitisation or allergy to latex can be identified in children up to five years of age." (my italics)
The study only examined children who were over one year of age, and states: "It cannot therefore be excluded that there were patients who were already sensitised at the age of one year." (my italics)
The report concludes: "Latex allergy occurs in children with no known risk factor for latex sensitisation".[28]
Conclusion
In spite of international research, no one has been able to explain why allergic diseases in childhood have increased so much in the latter half of this century.
Epidemiological thinking today is that early life exposure to allergen is more likely to lead to sensitisation than at any other time in life. Researchers are examining the effects of many possible culprits: house dust mite, cow's milk, wheat, pollens, cat epithelium, and many more. Unless latex and the chemicals used in glove manufacture are included, such research will be incomplete.
The upward spiral continues, and the number of atopic children has more than doubled in the past ten years alone. One in five children now have either asthma or eczema in childhood. Many babies today seem to be born with eczema or asthma, or to develop it within a few days of birth.
Asthma and eczema are known clinical reactions to latex allergy, but it is possible that other allergic diseases might be traced to the same source. Sensitisation to any allergen renders the individual prone to hypersensitive reactions to other, unrelated substances, and the symptoms of allergic disease can be manifest in any system of the body, including the brain.
Pre-powdered latex gloves have been in use for about thirty-five years. A whole generation has been exposed to them at birth, possibly sensitising many children who are now adults and having children of their own. It is well known that the atopic tendency runs in families.
The question must therefore be asked: are babies sensitised and develop the atopic condition by exposure to a powerful allergen at birth? or were they atopic in the first place and latex and chemical exposure at birth triggers the early development of allergic disease?
The Niggerman Report[27] states:
"While it is well known that the atopic disposition plays a key role in developing sensitisation and clinical symptoms to latex allergy, there is no information about the beginning of sensitisation and the risk factors during the first years of life." (my bold)
The evidence is in keeping with the hypothesis that neo-natal exposure to latex from gloves worn at the time of delivery may be a significant sensitising exposure.
The Way Ahead
Research is needed. But more practical and more effective would be a ban on the use of pre-powdered latex gloves in maternity units. I call upon the Royal College of Midwives and the Royal College of Obstetricians to take action. Other groups such as the British Asthma Campaign or the Anaphylaxis Group could also act. Self-help groups, such as these, which are usually run by lay people, can be very influential.
Thousands of babies have severe asthma and eczema in the first weeks of life. Anaphylactic reactions are becoming more common. If there is the slightest possibility, even though it is unproven, that latex exposure at birth could be partly responsible, these gloves should be removed from use in maternity hospitals immediately. The risk is otherwise too great.
Action Against Allergies Note
We believe this hypothesis to be without precedent. The author makes it clear that there is no proof to substantiate her theory, but its very plausibility is compelling, and calls for research. The only real way to validate or disprove the theory would be an epidemiological study, but in the first place review is necessary. Jennifer Worth has been invited by the British Asthma Campaign to apply for a research grant. She has also been asked by the Cochrane Airways Group, and the Cochrane Skin Group to undertake a systematic review study. For personal reasons, she can undertake neither. Any research student who could follow up these offers is invited to contact AAA.
Parliamentary Motion
* In a recent Parliamentary Motion read by Frank Cook, the House applauded the achievement of Jennifer Worth in securing first prize in the Action Against Allergies annual essay with this hypothesis, and commended her highly on this most original rationale and very pertinent set of propositions. There was some alarm that no programmes of enquiry appear to be underway in the study of neonatal response to this stimulus, and the Secretary of State for Health was urged to promote as a matter of urgency epidemiological research into this field of enquiry.
References
1. Booth B, Thomas L, Thompson G, Raune-Morris M, Lawton S. Nursing Times Special Report. Glove Allergies 1996.
2. Coombes RR, Gell PG, Clinical Aspects of Immunology. Blackwell, Oxford 1963 ch. 13.
3. Poole CMJ. Hazards of Powdered Surgical Gloves. Lancet 1997; 350 (9083) pp 973-974.
4. Beezhold D, Beck WC. Surgical Glove Powders Bind Latex Antigens. Arch. Surg. 1992; 127; pp1354-57.
5. Newson SWB, Shaw M. A Survey of Starch Particle Counts in the Hospital Environment in Relation to the use of Powdered Latex Gloves. Occup Med. 1997; 47; pp 155-158.
6. Anthony H, Birtwhistle S, Eaton K, Maberley J. Environmental Medicine in Clinical Practice. BSAENM Publications, Southampton. 1997. p335.
7. Jarrett EE. Activation of IgE regulatory mechanisms by transmucosal absorption of antigens. Lancet 1977 ii. pp 223-225.
8. Barnes PJ, Grunstein MM, Leff RR, Woolcock AJ. 1997 Asthma Volume II, Lippincot- Raven. p 1407.
9. Conybeare JJ ed. Textbook of Medicine. Sixth Edition 1942, Livingstone (Edinburgh). pp589-653.
10. Christie Brown R, Gilbert B, Fraser DB, Dobbs RH. Midwifery Fourth Edition 1956. pp 763-788. Edward Arnold (Publishers) Ltd.
11. Sussman GL, Beezhold DH. Allergy to Latex Rubber. Ann Intern Med 1995; 122; pp 43-46.
12. Novembre E, Bernardini R, Brizzi I, Bertini G, Mugnaini L, Azzari C, Vierucci A. The Prevalence of Latex Allergy in Children seen in a University Hospital Allergy Clinic. Allergy 1997; 52; pp 101-105.
13. Posch A, Chen Z, Wheeler C, Dunn MJ, Raulf-Heimsoth M, Baur X. Characterisation and identification of Latex Allergens by Two Dimensional Electrophoresis and Protein Microsequencing. J Allergy Clin Immunol 1997; 99; pp – 385-395.
14. Brehler R, Theissen U, Mohr C, Luger T. "Latex-fruit Syndrome": Frequency of Cross Reacting IgE Antibodies. Allergy 1997; 52; pp402-410.
15. Brostoff J, Gamlin L. The Complete Guide to Food Allergy and Intolerance. Bloomsbury. 2nd edition 1992. pp 302-305.
16. Ewan PW. Prevention of Peanut Allergy. The Lancet 1998; 352; pp 4-5.
17. Tariq SM, Stevens M, Matthews S, Ridout S, Twisleton R, Hide DW. Cohort Study of Peanut and Tree Nut Sensitisation by Age of 4 Years. BMJ 1996; 313; pp 514-517.
18. Ewan PW. Clinical Study of Peanut and Tree Nut Allergy in 62 Consecutive Patients: New Features and Associations. BMJ 1996; 312; pp 1074-1078.
19. Hatahet R, Kirch F, Kanny G, Moneret Vautrim DA. Sensitisation to Peanut before 4 Months – Based on 125 Cases. Rev Francais d'Allergol d'Immunol Clin 1994. 34; pp 377-381.
20. Hourihane JO, Kilburn SA. Clinical Characterisations of Peanut Allergy. Clin Exp Allergy 1997; 27; pp 634-639.
21. Fuchs T, Spitzauer S, Vente C, Hevler J, Kapiotis S, Rumpold H, Kraft D, Valenta R. Natural Latex, Grass Pollens, and Weed Pollen Share IgE Epitopes. J Allergy Clin Immunol 1997; 100; pp 356-364.
22. Bandolier. Special Bulletin for NHS Supplies 1994.
23. EEC Report 1997. Pollution Related Diseases in the Eurpoean Community. Brussels, COM (97); 266; 97/d 153 (COD) 4.
24. Anthony H, Birtwhistle S, Eaton K, Maberley J. Environmental Medicine in Clinical Practice. BSAENM Publications, Southampton. 1997. pp 80-103.
25. Booth B. Natural rubber (latex) allergy Part II Nursing Times 1994; 90; pp 30-32.
26. Cremer R, Hoppe A, Kleine-Diepenbruck U, Blaker F. Longitudinal Study on Latex Sensitisation in Children with Spina Bifida. Paediatric Allergy Immunol 1998; 9; pp 40- 43.
27. Niggerman B, Kulig M, Bergmann R, Wahn U. Development of Latex Allergy in Children up to 5 Years of Age – A Retrospective Analysis of Risk Factors. Paediatric Allergy Immunol 1998; 9; pp 36-39.
28. Sorva R, Makinen-Kiljunen S, Suviletho K, Juntunen-Backman K, Haahtela T. Latex Allergy in Children With No Known Risk Factor for Latex Sensitisation. Paediatric Allergy Immunol. 1995; 6; pp 36-38.
Comments:
-
No Article Comments available