Positive Health Online
Your Country

Nursing at the Royal London Homoeopathic Hospital NHS Trust
listed in nursing, originally published in issue 43 - August 1999
The Royal London Homoeopathic Hospital (RLHH) is unique as it provides the only service in Europe which is dedicated to complementary medicine as an integral part of the National Health Service (NHS). Becoming a 3rd wave NHS Trust in 1993, focussed our existence and care delivery purely towards complementary medicine. The RLHH has been a part of the NHS since its inception in 1948. The fact that complementary medicine is available within the NHS is however, probably one of the best-kept secrets.
The name of the hospital slightly misleads the reader as to the therapies practised. The multidisciplinary team at RLHH aims to offer the patient a holistic approach to care in order to meet individual needs. It does this by offering a range of therapies, which include: homoeopathy, acupuncture, manipulative medicine, nutritional medicine, autogenic training, relaxation techniques, reflexology, aromatherapy and massage to name but a few. The RLHH provides care for individuals with a wide range of conditions using therapies which are complementary to conventional medicine and not as an alternative. The ultimate aim of this integrative approach is to enhance patients’ health.

A nurse applying acupuncture to a patient.
It is increasingly evident that the role of the nurse in today’s health care system is diverse, and in many ways defies definition, however, nursing could be described ‘generically’ as a way of promoting both the health and well being of an individual (Rogers, 1970, cited in Swift, 1994). Nurses are developing their skills, not only in technical terms, but also to augment that definitively elusive concept of ‘caring’.
Much of the approach to nursing at RLHH is comparative to other general medical units. However, within the multidisciplinary team the nurses’ and therapists’ role is key to the delivery of the ‘hands-on’ therapies. Nurses by tradition have a strong background in ‘caring’. The introduction of ‘hands-on’ or touch therapies alongside mainstream care has developed the therapeutic role of the nurse and further enhanced our patient care.
The potential for nurses to extend their therapeutic role in this area has been recognised, and the challenge of integrating complementary approaches to care is seen as the way ahead for the nursing team. In the RLHH nurses and therapists are ideally placed to promote a skilled and quality complementary care service that meets the patients actual requirements.
In recent years many changes have occurred within the National Health Service (NHS), and the RLHH has not escaped these, including the expansion of the nurses’ role which increases the ‘scope’ of professional nursing practice (Koldjeski, 1993). The use of complementary therapies as routine for our inpatients and the setting up of nurse-led outpatient clinics is such an example. However, the use of complementary therapies is not seen as “just another treatment” (Sayre-Adams & Wright, 1995). The nursing team believe that the use of such therapies allows the “healing potential, the consciousness and intention of the nurse” to be expressed (Sayre-Adams & Wright, 1995), meaning that the very consciousness and awareness of the practitioner is paramount to the delivery of care, not just delivering complementary therapies.
It is not only nurses who are seeking to add another dimension to their caring role. The patients too, would also appear to be changing, in that they play a more active role in seeking out appropriate or preferred methods health care. Patients will very often seek out complementary therapies following a failure or dissatisfaction with conventional medicine (Lynn, 1996), or because they have found that using a particular therapy or therapies has been useful in their quest for health. It may also be that the underpinning philosophies of many of the therapies hold more meaning to the individual than the complex world of ‘modern medicine’. As Kushi (1981) points out of complementary therapies: “Instead of complexity, they offer simplicity. Abandoning the artificial, they stress the natural. The purpose is to unite the scientific knowledge that modern man has acquired with the intuitive knowledge that man once enjoyed.”
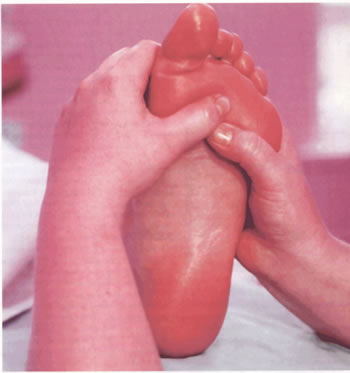
Reflexology
Touch therapies have been viewed as a natural extension of nurses’ role (Sanderson and Carter, 1994). The importance of non-verbal forms of communication including massage and touch has also been highlighted by a variety of authors (Corner, Cawley and Hildebrand, 1995; Carter, 1995).
The benefits of touch therapies on the psychological well being of the individual have been well documented. Research has shown that touch produces a reduction in anxiety levels, particularly in those groups unaccustomed to touch in their daily life (Thomas, 1989).
It is evident from the numbers of referrals received at the RLHH that there is an increasing awareness and demand for our services. There is also an increasing interest in complementary therapies being shown by nurses. The move towards integrating complementary therapies in nursing would also suggest that care delivery is increasingly being seen as a less passive process, and more of a dynamic development (McMahon, 1991). Indeed, the term ‘therapeutic’ nursing has only recently begun to be used to promote this approach within nursing care.
The ‘therapeutic’ nursing activities at the RLHH is seen very much as Hockey (1991) describes them, in that the delivery of these therapies have a healing effect, or result in the patient moving towards healing or wellness.
This approach, enhances the notion that nursing is a concept which is holistic and therefore, necessary for the total health of the individual who is receiving the care.
There are many issues involved in the integration of complementary therapies into our nursing practice. These issues concern ensuring a high quality care, safe practice and that any use of a complementary therapy has an effect on the outcome and quality of life of the receiving person.
The RLHH has an active programme of clinical audit. Some of the work carried out has involved the use of audit cycles to ensure that clinical care is of the highest possible standard. More recently, the primary focus has been the evaluation of the outcome of treatment offered at the hospital.
Presently, many health care decisions remain opinion based. That is based on values and the resources available. Until recently little attention had been paid to the evidence for care delivery based on research. There is a distinct move towards providing widespread evidence based medicine. Evidence based medicine is where clinical and managerial decisions are based on the best possible evidence. Sackett (cited by RLHH, 1997), has described the process as:
• Asking a focused questionThe current interest and pressures on resources has changed the onus of decision making. Those who take decisions need to be able to produce and describe the evidence on which the decision was based. This still remains the case even when the evidence is difficult to find or poor in quality. Thus as the pressure on the resources increases, there will be a transition from opinion based decision making to evidence based decision-making.
• Finding the evidence
• Appraising the evidence
• Acting on the results
• Appraising one’s own performance.
To accomplish this, the best available evidence relating to a particular decision must be found. It is arguable whether the skills necessary to evaluate the evidence for complementary therapies are present in the current health care system. The knowledge of such therapies may not be there in the first instance, and the research to support such therapies, particularly in randomised controlled trials, have been both rare, and in many cases of poor quality (Vickers, 1996).
As stated the ethos of the hospital is to provide complementary medicine with a patient focussed approach. Both chronic and acute conditions can be distressing and debilitating and leave the patient feeling isolated. The necessity to attend a hospital, despite the relief gained by doing so, can for many prove to be an additional isolating and dehumanising experience (Beckwith, 1993). It could be argued that the need for touch therapies might be greater in a different, unfamiliar and occasionally isolating environment.
Within the context of the integration of complementary therapies, it is seen as essential that the potential benefits of the therapy employed be understood, and that they are discussed and conveyed to the patient and to all other relevant team members.
From a psychological perspective ‘touching with intent’ (White, 1988) is described as having the ability to reduce the patients feeling of isolation. Even hospitals with the prime objectives of holistic care can have an isolating effect on a person, and the use of touch can be a powerful tool within this environment. Beckwith (1993) discusses touch as a form of communication, socialisation and caring. Feltham, (1991) also discusses touch in these terms, but focuses more on touch in the context of dependency, altered body image, lowered self esteem and anxiety, believing that touch can help in these instances. Patients attending RLHH present with varying forms of all of the above-mentioned psychological issues, some of which may compound or exacerbate the physiological symptoms. The use of touch therapies alongside other support has been found to be useful.
The aim of any nursing intervention is to maximise the individuals’ chances for optimum function and independence. At all stages, the nurse has to take into consideration the patients’ wishes, motivation, habits, roles and the physical, social and cultural environment in which they live and work. Assessment of patients takes place through observation, interview and assessment of their physical abilities and level of independence. Treatment or intervention could therefore, encompass a variety of methods or techniques.
An advance in nursing practice involves breaking new ground and exploring new boundaries. Any development can be positive, provided it is patient focussed and practices within the nurses professional boundaries (Gee, 1995). Complementary therapies are most definitely patient focussed, and have the added advantage of not requiring expensive equipment, provision of a large area to practice, and can be incorporated within many existing clinical roles.
A systematic analysis of the quality of the complementary therapy service can play a valuable developmental role. The careful use of audit can evaluate the resources, adherence to protocols, resulting outcomes and provide feedback on the relationship between the service and its objectives. An effective audit can assist in providing reassurance to other team members of the quality and benefits of the service. It can also provide a baseline data to negotiate for increased resources (Vickers, 1996; Milne and Learmonth, 1991).
The success of any audit is in part dependent upon the accurate recording of data, including outcome goals. Outcome goals would be identified in documentation as evaluation of intervention. This information can be obtained via several methods including simple questioning of the patient, using recognised and accepted methods, such as rating scales for pain and relaxation, simple questioning of the patient and subjective feedback questionnaires.
On setting up the nurse-led outpatient clinics, the nurses elected to view the outcome of their treatments from the patients’ perspective, and have modified an approach initially used in Primary Care known as Measure Yourself Medical Outcome Profile (MYMOP). The nurses at RLHH believe they should evaluate the outcomes of their interventions as Kemp and Richardson summaries (1990, cited in Higgins et al, 1992). Three main reason for doing so are:
• A way of ensuring that the client, nurse and profession are satisfiedGaining skills and using complementary therapies adds another dimension to nursing intervention, and may also be extremely rewarding for the therapist. Incorporating complementary therapies into treatment programmes enhances both the philosophy of care, and patient empowerment.
• To check that valuable resources are being used effectively
• The results of an outcome measurement can increase the nurse’s knowledge and enhance the public’s confidence in the profession
As the use of complementary therapies is an additional skill for the nurse, it is essential that they be used within the boundaries of the profession. The benefits of incorporating complementary therapies into practice are many. They broaden the skill base of the nurse, and fit well into general role of the nurses within many areas.
Complementary therapies have successfully been integrated into our programmes of care, and relaxation techniques and elements of the therapies have been taught to patients as a form of self treatment, or to their carers as a way of being able to provide another approach to their care. Thomas (1989) identifies in his study that most nurses engaged in carrying out complementary therapies such as reflexology saw the technique as a useful intervention. By the skilful use of touch, nurses can relieve pain, give comfort and aid relaxation. The practice of complementary therapy can be as refreshing for the practitioner as well as the client. Interaction between the hands of the giver and the skin of the receiver can assist in opening up two way communication, create therapeutic bonds, whilst at the same time retain appropriate boundaries.
In conclusion, recent years have seen many changes occurring within the NHS, including the emphasis on evidence-based practices, clinical outcomes and the expansion of the nurses’ role.
Touch is essential for optimum health, early physical and emotional development, emotional release and in creating feelings of security and love (Stormer, 1992). It is hoped that further evidence of the success in integrating complementary therapies will continue to see an improvement in the patients’ wellbeing. It is however, important to remember that in order to bring innovation to practice, nurses must let go of preconceived ideas in regard to their limitations of practice (Adamson and Harris, 1995). Adamson and Harris go on to quote Florence Nightingale: “Nurses should use well every power they have”, a philosophy that could easily be transposed to the use of complementary therapies today. However, the integration of these therapies within the profession of nursing should be against the backdrop of the professional code of conduct, with assurances of the highest standards and professionalism in their delivery.
References
Adamson, S. Harris, E. 1995 Reflexology in nursing practice. Nursing Times. 9(2).Beckwith, C.A. 1993 The concept of touch as an aspect of therapeutic nursing. Complementary Therapies in Medicine. Vol 1 pp 211 – 214.
Carter, A. 1995 The use of touch in nursing practice. Nursing Standard 9(16) pp31–35
Corner, J; Cawley, N.; Hildebrand, S. 1995 An evaluation of the use of massage and essential oils on cancer patients. International Journal of Palliative Nursing. 1(2) pp 67–73.
Hockey, L. 1991: Foreword in McMahon, R. & Pearson, A. (eds.) Nursing as Therapy. London, Chapman and Hall.
Feltham, E. 1991 Therapeutic touch and massage. Nursing Standard 5(15) pp26–28.
Gee, K. 1995 Competency through being: The enemy within. British Journal of Nursing 4(11) pp637–640.
Higgins, M.; McCaughan, D; Griffiths, M; Carr-Hill, R. 1992 Assessing the outcomes of nursing. Journal of Advanced Nursing. Vol 17 pp 561–568.
Koldeski, D. 1993 A Restructured Nursing Process Model. Nurse Educator. 18(40) pp33–37
Kushi, M. 1981 Information Leaflet. The Michio Kushi Institute of Great Britain, London.
Lynn, J. 1996 Using complementary therapies: Reflexology. Professional Nurse 11(11) pp 321–322
McMahon, R. 1991 Therapeutic Nursing: theories, issues and practice in: McMahon, R. & Pearson, A. (eds.) Nursing as Therapy London. Chapman and Hall.
Milne, D. Learmonth, M. 1991. How to evaluate an occupational therapy service: A Case Study. British Journal of Occupational Therapy. 54(2) pp42–44.
Rogers, 1970, quoted in Swift, G. 1994. A Contextual Model for Holistic Nursing Practice. Journal of Hospital Nursing 12(3) pp 265 – 281
Sackett, D. 1997 cited in The Evidence Base for Complementary Medicine. RLHH, p 5
Sayre-Adams, J. Wright, S. 1995. Change in Consciousness. Nursing Times. 91(41)
Stormer, C. 1992 Reflexology. Hodder and Stoughton. London
Thomas, K.B. 1987 General Practice Consultations: Is there any point in being positive? British Medical Journal. 294 pp 1200 – 1202.
Vickers, A.J. 1996 Massage and Aromatherapy: A guide for health care professionals. London. Chapman and Hall.
White, J. 1988 Touching with intent: Therapeutic Massage. Holistic Nursing Practice 2(3) pp 63–67.
Comments:
-
No Article Comments available