Positive Health Online
Your Country

The Real Causes of IBS: How they can be Revealed by Comprehensive Digestive Stool Analysis
by Michael Franklin(more info)
listed in ibs, originally published in issue 121 - March 2006
IBS (Irritable Bowel Syndrome) is a mixture of any two or more of the five following symptoms: constipation, diarrhoea, abdominal pain, flatulence and bloating. Broadly speaking, these symptoms need to have existed for at least three to six months before a diagnosis of IBS can be made. If they have lasted only a couple of weeks, for example, a more likely cause is a simple stomach bug or minor gastrointestinal upset.
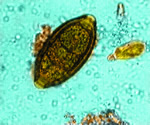 Trichiura |
 pictured inside a patient's gut |
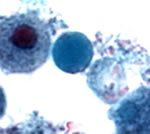
 Blastocystis hominis |
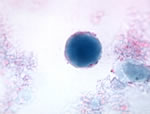
 Entamoeba histolytica |
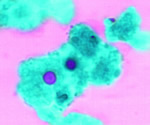
 Giardia lamblia |
 Candida albicans shown atta- ched to the villi on the gut wall |
The big problem with IBS is that its treatment by orthodox medicine is usually inadequate. When a patient goes to a GP with IBS-type symptoms, the GP will only be concerned and will only refer the patient to a gastroenterologist if he thinks there is a chance the patient may have either advanced stages of cancer, or ulcerative colitis or Crohn's disease. (These are what a specialist is looking for when he does an endoscopy or sigmoidoscopy or colonoscopy for someone with IBS-type symptoms). GPs know that colon cancer is much more likely if you are over 50 and that Crohn's or ulcerative colitis (jointly known as inflammatory bowel disease or IBD) usually start in the 20s. So they will have those considerations very much in their mind when it comes to deciding whether to refer a patient or not.
If nothing is found by any of the above tests, or by a barium meal, which tests for much the same thing, or by a test for coeliac disease, the consultant will simply tell the patient he or she has IBS and refer them back to their GP with the implication that nothing much can be done. Either the consultant or their GP tells them they will simply have to live with it.
Surely there must be a better way to help people with IBS? I first started seeing patients as a clinical nutritionist in 1989 and I always knew that a fair number of IBS cases could be solved by pinpointing each patient's individual food intolerances. But there were some cases in which no matter how many foods a patient eliminated or how much they fiddled around with their diet, they did not get any better.
Then along came news that a test which had been used very successfully in America could now be made available to our patients in England. With its help everything instantly became clearer. Those patients who did not see a significant reduction in their symptoms after changing their diet could have their stools analyzed by sending them by special air mail to an American laboratory and parasites, unfriendly bacteria or yeast overgrowth were revealed to be an additional cause. Once we started using the test, we found we were getting major improvement in almost all of our IBS patients.
In the Autumn of 2005 we decided to analyze the results of 120 patients who had done this test with us. The main findings are shown on the following pages.
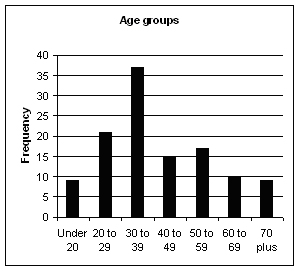
Figure 1
It can be seen from the above that, of the total sample, 63% were female and 37% male (See Table 1 and Fig 1) which reflects the usual assumption in medical circles that IBS is roughly twice as common in women than in men. As far as age is concerned, 7.5% were in their 70s, which shows that age should not be a barrier when it comes to having the determination to seek the cause of a long, chronic illness. Remarkably, two of these patients were women, both aged 73, and both had had IBS for 40 years. Both turned out to have parasites and no doctor or practitioner had ever previously looked for these as a cause of their IBS.
Another 7.5% of the patients were under 20 (See Table 2) and I can add a personal observation here. Every single one of those turned out to have parasites or a high amount of unfriendly bacteria – which suggests that if a teenager has been complaining of IBS for months or years they should be taken very seriously.
Parasites
31.6% of those who did the test turned out to have parasites. They are especially likely to be a cause where the major symptoms are:
- Diarrhoea or endless loose bowel movements
- Abdominal pain
- A lot of gurgling or churning accompanied by the first two symptoms
If the origin of the symptoms can be traced back to a bad stomach upset experienced in foreign travel, it increases the likelihood of parasites as a cause. India, Nepal, Egypt, the Dominican Republic and Turkey seem to be the most problematic destinations – in that order! But we have found some patients with parasites who have never travelled outside Britain, so foreign travel is not always the cause. (See Table 3).
Blastocystis hominis, pictured top of page, was the parasite found most frequently. Twenty two% were harbouring it in their colon and 12.8% had Dientamoeba fragilis.
The parasite which is named in most health books about the gut and digestion is Giardia lamblia. (See page 26). But it did not occur once in the 120 tests we had analyzed. That's interesting because it suggests (a) that it is very uncommon in Britain and (b) that readers should be aware of generalizations found in bland books on health where the authors have not done their homework.
Where parasites are found, certain herbs such as Artemesia annua can be helpful but probably only if the parasite is not Blastocystis hominis, which can be very hard to eradicate or if, in the case of Dientamoeba fragilis, the patient has a number greater than that which the laboratory classifies as 'rare'. In cases of B. hominis or where a significant amount of D. fragilis is found, the appropriate anti-parasitic drug is probably the only answer.
Beneficial Bacteria
The phrase 'beneficial bacteria' means the same, broadly speaking, as 'friendly gut flora' or 'probiotics'. The two most important are Lactobacillus acidophilus and Bifidobacteria and these are measured on a scale of 0-4 by the CDSA test. These are just two of the friendly bacteria which are found in natural, organic yoghurt. These friendly bacteria are very beneficial to intestinal health and the ever-growing number of medical trials which have found them helpful are why, just in the last few years, commercial yoghurt makers have entered the market to try and persuade us all to eat yoghurt with these friendly bacteria added. Unfortunately, certain commercial yoghurts are not recommended by experts in gut health because they may contain a significant amount of added sugar, an ingredient which tends not to help gut health in general and which is particularly bad for those already suffering from yeast overgrowth or 'Candida'. (See Tables 4-6; Figures 2-4).
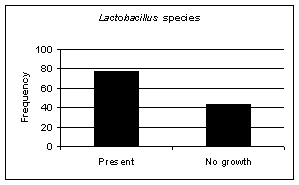
Figure 2
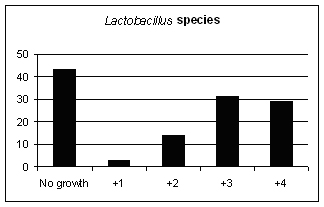
Figure 3
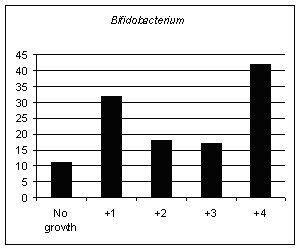
Figure 4
Yeasts
50.8% of patients showed some growth of yeast. This is an area which has been the subject of a great deal of discussion, misunderstanding and controversy ever since an American doctor from Alabama who specialised in psychiatry called Dr Orian Truss published three papers about it in the Journal of Orthomolecular Psychiatry and followed them with his own self-published book on the subject, The Missing Diagnosis, in 1983. Truss reported in his papers and his book how he had found Candida to be the cause of many diverse symptoms such as bloating, flatulence, constipation, diarrhoea and vaginal and oral thrush, and to be associated with skin conditions such as eczema and urticaria and 'mental' symptoms such as extreme mental fatigue and an inability to think clearly. Truss ascribed the problem to Candida albicans, but he would have been more accurate had he used the phrase which some enlightened doctors have used: yeast overgrowth. That is because, as the CDSA test reveals, the yeasts identified in some people's guts is not always Candida albicans, but can be of several different species (See Tables 7-8 and Figures 5-6).
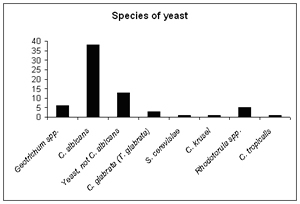
Figure 5
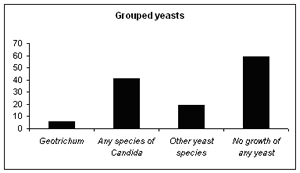
Figure 6
Geotrichum and Rhodotorula are described by Great Smokies Diagnostic Laboratory, the founders of the CDSA test, as "rare, opportunistic organisms usually isolated only in immunocompromised hosts". As Table 8 shows, our analysis showed Geotrichum in 5% of cases and Rhodotorula in 4.2%. Were these patients immunocompromised? I would say that, based on consultations with them and question-naires that they filled in, none of them were severely immunocompromised or even considerably immunocompromised. But there is no doubt that their health was not particularly good and they presented with a large number of different symptoms. So it does suggest that where Geotrichum or Rhotodorula are found, the patient's intestinal health will be far from good.
The good news is that all these causes are treatable, whether they be parasites, unfriendly bacteria, lack of beneficial bacteria or yeast overgrowth.
The important thing is to identify which particular cause or causes are applicable in each individual patient. In many cases – and this is the most important thing to grasp about IBS – two, three or even four of these causes are all present in the same person. Unfortunately, people seldom look at more than one. That's analogous to having four nails in your shoe. If you only get rid of one of them, it will still hurt to walk!
References:
Truss, Orian. Tissue injury induced by Candida albicans: mental and neurologic manifestations. The Journal of Orthomolecular Psychiatry. 7 (2): 1978.
Truss, Orian. Restoration of immunologic competence to Candida albicans. The Journal of Orthomolecular Psychiatry. 9 (4): 1981.
Truss, Orian. The role of Candida albicans in human illness. The Journal of Orthomolecular Psychiatry. 10 (4): 1983.
Truss, Orian. The Missing Diagnosis. Birmingham, Alabama 1983.
Madden, J. and Hunter, J. A review of the role of the gut microflora in irritable bowel syndrome and the effects of probiotics. British Journal of Nutrition. 88: (Suppl. 1), s67-s72. 2002.
Hamilton-Miller, J. Can probiotics improve health? Pulse. 60(6): 53,57. 2000.
King, T., Elia, M., Hunter, J. Abnormal colonic fermentation in irritable bowel syndrome. Lancet. 352: 1187-9 1998.
Young, R., Vanderhoof, J. Successful probiotic therapy of chronic recurrent abdominal pain in children. Gastroenterology. 112: A856 1997.
Comments:
-
No Article Comments available