Positive Health Online
Your Country

Candida: Diagnostic and Therapeutic Approaches
listed in colon health, originally published in issue 62 - March 2001
Introduction
There is, and has been for many years, a tendency for alternative practitioners to diagnose anyone suffering from a wide variety of unexplained symptoms as suffering from 'Candida'. Numerous magazine articles, largely written by unqualified authors, have for years told us how Candida has 'infected all of our internal organs' or that it is in our 'blood, circulating around our bodies'. This has led to the myth that an individual suffering from 'Candida' is a giant fungal ball with their entire intestinal tract full of Candida. It will not surprise (I hope) many practitioners, however, that this is complete medical nonsense, with absolutely no scientific fact at all. However, before we decide that there is therefore no such thing as 'candidiasis' it is important to emphasize, as anyone treating such patients will point out, that a great many individuals with such symptoms will respond, in some cases dramatically, to antifungal and anti-Candida diet regimens, and that undoubtedly such a syndrome, or syndromes, does exist and affects an increasing number of individuals.
The History of Candida
Before we can discuss the truth about Candida, it is important to know how the concept of a widespread Candida infection (candidiasis) has come about. Such a hypothesis was first described by Dr Orian Truss in 1978.[1] His work was then extended by Dr William Crook, who has probably done most to popularize the Candida hypothesis.[2] Since then it has become big business, with a wide variety of practitioners ready to diagnose such a condition by a wide spectrum of 'alternative means' and supplement companies ready to provide us with a bewildering array of supplements and 'natural products' that claim to have anti-Candida properties. However, in the 23 years since Truss's description of this condition there is still a great deal of controversy surrounding exactly what it is; indeed, there is much evidence that what he was probably describing was a collection of syndromes, all related to a weakened immune system, and the resulting imbalance in our natural flora.
Who Gets Candida?
There is little doubt that the single most widespread cause of candidiasis is the indiscriminate administration of broad-spectrum antibiotics. In addition to their desired effect, they also kill off commensal (resident) bacteria in the gut. This 'flora' is vital for optimum health and proper gut function. A reduction leads to the overgrowth and increased pathogenicity of other micro-organisms such as the Candida species. A number of other factors also seem to predispose an individual to Candida infections. In cancer patients, especially those who have had chemotherapy, fungal infections have always been a major problem. A similar effect is seen in HIV patients who not only suffer recurrent Candida albicans infections but infection with other species such as Candida krusei and Candida glabrata, which can often be more resistant to antifungal therapy. Immunodeficiency associated with long-term debilitating illness may also be accompanied by such infections, such as the chronic fatigue syndromes and diabetes. Other factors include the use of steroids – arthritics and asthma patients are particularly prone – and hormone treatments such as the contraceptive pill. These are the facts that will have a fairly universal agreement within the medical profession. However, many patients seen with candidiasis do not fall neatly into these categories. This is where the controversy comes in. Most of us who have tested and treated many of such patients believe that other environmental factors can lead to a degree of immunodeficiency, providing a suitable environment for a fungal-type dysbiosis to occur. These include poor adrenal function, a diet high in refined sugars, poor nutrition, surgery, particularly gastrointestinal, and other diseases. Even more controversial is the possibility of generations of damaged immune systems by radiation from nuclear testing and widespread vaccination programmes.
What is Candida?
Candida albicans is a natural part of our flora, i.e. it is a commensal organism. It is a yeast that is present in our intestinal tract, skin and the genito-urinary tract. In this form it is an important part of the very fine balance of micro-organisms that exists for our health. However, Candida can change into a pathogenic form (disease causing), a filamentous fungal form, which can extend out small threads called hyphae into the surrounding cells. It has been postulated that it is these hyphae that provide a route for increased permeability across the gut wall, leading to the so-called 'leaky gut syndrome', which is an important part of the aetiology of this condition. It is also known that Candida can secrete a number of powerful toxins into the surrounding tissues and ultimately the bloodstream. It may be that many of the symptoms associated with Candida could be due to the action of such toxins rather than the Candida itself.
What is Candidiasis, and How Does It Come About?
This is the most difficult question of all to answer, at least with any degree of consensus of opinion. One of the more recent attempts by respected bodies such as The British Society for Allergy Environmental and Nutritional Medicine (BSAENM) to describe this syndrome or syndromes has been to classify it as fungal-type dysbiosis, based on the currently available evidence, mainly in the light of insufficient data to confirm that Candida albicans is always the only cause. This refers to a relatively common condition, which responds to antifungal agents and the avoidance of fermentable foods. The facts regarding a fungal cause are as follows:
*It is frequently associated with endogenous ethanol production on sugar challenge: such fermentation is regarded as predominantly a yeast phenomenon;[3]
* Removal of fermentable foods from the diet reduces both symptoms and ethanol levels;
* The syndrome responds to antifungal drugs;
* Antibacterial antibiotics make it worse;
* Oral and vaginal thrush are much more common in patients with the syndrome than in the population generally.[4]
Further evidence for the fungal connection comes from the patients' histories themselves. These individuals often react to foodstuffs containing yeast or mould (bread, wine, mushrooms etc); they are often made worse by mouldy or musty surroundings, with evidence of inhalant allergy reactions, and there are often accompanying fungal infections, including athlete's foot and other skin infections.
The diagnosis and the exact mechanism behind how such a fungal-type dysbiosis causes its symptoms are further hampered by a number of factors that are inevitably associated with the syndrome:
* The condition seems to predispose to food allergy (type B or sensitivities) and vice versa;
* Absorption of nutrients is commonly compromised, leading to nutrient deficiencies, which may cause further evidence of dysfunction;
* There may also be increased permeability[5] of the gut, allowing the passage of larger molecules;
* Increased gut permeability often accompanies food allergy and fungal-type dysbiosis, but the possibility that increased permeability may be a primary anomaly cannot yet be excluded;
* The normal interactions between the gut contents and the host have not been established in detail.
This has led to a great deal of difficulty in correctly identifying patients who have Candida as their primary problem, since also many symptoms may result from both deficiencies and excesses and there is a wide individual variation in the presenting symptoms.
Diagnosis of Candidiasis (Fungal-type Dysbiosis)
We have been plagued for many years, since the concept of Candida being involved in such syndromes in fact, by the lack of reliable laboratory investigation techniques to diagnose the condition correctly. This has led inevitably to a whole host of 'alternative techniques' being used, which have little or no scientific basis. This not only inevitably leads to a wrong diagnosis, but is at least partly to blame for the lack of acceptance by the medical profession as a whole. Many practitioners have had to rely on a detailed symptom questionnaire, but for all of the reasons already mentioned, such an approach is wholly unreliable, and often reflects an individual under stress rather than any single specific condition. A number of laboratory investigations have, however, become available, the most important of which are as follows:
Gut Fermentation Tests
A resting blood alcohol level is measured, then a second sample is analysed after ingestion of a sugar dose. If alcohol appears in the blood, this suggests fermentation is going on. The test has been further refined to look for a number of different fermentation products. However, it does not give any information regarding what is doing the fermenting, as there is increasing evidence that many bacteria can provide such a fermentation reaction. In our experience this type of test is not always positive for individuals with a confirmed Candida infection.
Candida Stool Culture Tests
Since Candida is present in the gut, it is possible to culture (grow it) from a stool sample. Using a special culture medium and the right anaerobic conditions (reduced oxygen), Candida can be grown and identified. Some laboratories go further to try to quantify the relative amounts of Candida present. This is, however, a very difficult and inexact procedure. The amount of Candida that grows is often more dependent on the culture condition than the amount present in the sample. Similarly there is no real evidence that Candida exists in any significantly increased amounts in such syndromes, and the mere presence of it in a stool would be meaningless, as we have already stated that it is present as a natural part of our gut flora. Many studies have tried to demonstrate such an increase in these fungal syndromes without success. However, some specialist laboratories are able to identify different species of Candida that should not normally be present, and such a result would therefore be significant.
Candida Urine Tests
Such tests look microscopically for the presence of Candida in a urine sample, in addition to a culture. However, Candida species would only be present in a urine sample if they had caused a local infection, i.e. vaginal thrush or a urinary tract infection, which would best be tested for by taking a swab from the infected area and a subsequent culture. This type of test therefore is not useful for detecting a widespread or systemic Candida-type reaction.
Candida Saliva ELISA Test
If Candida has become pathogenic, i.e. disease causing, it will elicit an immune response. One of the effects of such a response will be the production of elevated levels of specific antibodies to in this case Candida. The technique used is called an ELISA (enzyme-linked immunosorbant assay), which is a very powerful and sensitive tool for the measurement of biological material, in this case antibodies. Briefly, Candida is chemically coated to the bottom of a special plastic plate (microtitre). The patient sample is diluted and incubated in this plate. If any antibodies that recognize the Candida are present in the sample they will strongly bind to the Candida; all remaining sample that is not bound can then be washed away. An anti-human antibody (that has been raised usually in a rat or goat), which has an enzyme chemically attached to it, is then incubated with the sample. This time if there are any anti-Candida antibodies present from the original sample the anti-human antibody that has been added will bind to them. Again, any unbound antibody is washed away, and a special substrate is added. This is simply a colourless solution that the enzyme attached to the anti-human antibody will cause to produce a coloured product. This colour can then be very accurately measured by a spectrophotometer. If appropriate standards are included, i.e. an exact known level of Candida antibodies, the colour that this produces can be used to produce a standard curve; a computer can then analyse the test sample's colour to give an exact value of how many Candida-specific antibodies were in the original sample.
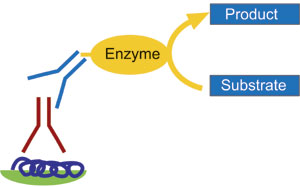
Enzyme-linked Immunosorbant Assay (ELISA)
With a further refinement of this technique by making the second anti-human antibody with the enzyme specific to a particular class of antibody, i.e. immunoglobulin G (IgG) and immunoglobulin A (IgA), two different types of Candida antibodies can be detected (see diagram). The importance of this is that the IgG-type antibodies tend to reflect a long-term or old infection, whereas the IgA class antibodies represent a more recent or active infection. Most recently in our laboratory we have been able to modify this test, to be performed from a saliva sample. This has the obvious advantage of not having to have a blood sample drawn. More importantly, since Candida is in essence an infection of the mucosal surface, saliva represents a more suitable medium for the detection of such infections than the blood sample. We have, for example, very recently seen IgA class antibody levels in excess of 90 times that seen in a normal population in a lady with a history of long-term antibiotic use, and recurrent bacterial and fungal infections. One of the major drawbacks with this approach is that in a small percentage of cases there is evidence of an IgA deficiency, which could lead to a falsely lowered reading or a negative result. This is compounded by the fact that such individuals are more likely to suffer from recurrent infections of the very nature that we are testing for! In our laboratories we have been able to study several thousand such individuals, with in excess of 90% demonstrating an improvement on an anti-Candida diet. It is our belief that this type of approach represents the most reliable means of detecting such Candida infections at the present time.
Therapeutic Approaches
There is no real consensus regarding the ideal treatment approach to these fungal-type dysbiosis syndromes, and this has at least in part contributed to the confusion and scepticism surrounding such infections as a whole. The arguments surround mainly the role of antifungal pharmaceuticals versus a more natural approach.
Diet
Here again there is variation in treatment plans. Practitioners in Sweden may exclude dairy produce as part of an anti-Candida routine; others in Britain may cut out all grains; others still may exclude all fruits. The basic tool on which there is almost universal agreement, is the use of a low-fermentable-food-based diet. A completely sugar-free diet is impossible to provide, but it should be as low in the fermentable sugars as possible: sucrose, glucose, and fructose should be eliminated, as well as natural sweeteners such as honey, corn syrup, maple syrup, rice syrup etc. There is a difference of opinion about lactose. Some yeasts can ferment it, so some practitioners prefer patients to reduce milk and dairy intake. We do not generally do so unless the patient also has a intolerance or an allergy to milk. Applied strictly, such a diet is usually effective in reducing symptoms within 1-3 months, but may have to be continued for long periods, with patients returning to it if they relapse.
Many practitioners also advise reducing the consumption of yeasts and all fermented foods. Some but not all patients with fungal-type dysbiosis are also intolerant of yeasts. From studies in our own laboratories, approximately 70% of patients have a demonstrable yeast sensitivity from blood tests. In practice, yeasts may be restricted at first and reconsidered after the patient has improved, reintroducing them if symptoms do not get worse after a challenge, or yeast restrictions may be recommended only to those who fail to improve on a less strict diet. Yeasts are inactivated in the human gut only by stomach acid, and may not be inactivated if stomach acid is low. They may be present as viable cells in the small bowel, and could be one of the causative organisms of fungal-type dysbiosis.
The consumption of mouldy foods should also be restricted, especially mouldy cheeses. Evidence for this is mainly again from experience, with patients often reacting to them. There are also problems with alcoholic drinks: this may relate not to any yeast content but to the fact that alcohol is metabolized much like carbohydrate, and numerous studies have demonstrated the effect of increased permeability of the gut by alcohol.
Following such a diet regime a number of patients report a worsening of symptoms for the first few weeks, which has been attributed to a reaction to killed yeast cells (Candida die-off). If the treatment programme is adequate, clear evidence of improvement is often seen within a month. Thereafter, the diet should be kept strictly for 3-6 months; occasionally longer. After about 3-6 months the patient can experiment by increasing carbohydrate intake (but not sugar) and introducing individual foods. Patients, however, differ in their tolerance of the individual foods: they should return to the previous stage at the first sign of deterioration. By this time most patients will have ceased to crave sugar: some can return to it, but for most it will never be safe to have more than small amounts.
Nutritional Supplements
The antifungal diet is nutritionally adequate, but most practitioners would add a multivitamin/multimineral supplement, plus any additional supplements indicated by nutritional testing (particularly B vitamins, zinc and magnesium.[6]
Supplements of Commensal Bacteria
Finally, it makes sense to try and recolonize the gut with 'friendly bacteria'. Most well known among these is Lactobacillus acidophilus, the yoghurt-making bacteria. Many supplements of 'acidophilus' are currently being marketed. Some contain very few live bacteria. A recent study reported that many of the products examined did not match their declared bacterial specifications and were either inactive or contained less than a tenth of the declared dose.[7] Live yoghurt has been used as a source of beneficial gut bacteria since the 1930s and clinically enough of the bacteria present will survive the acidity of the stomach to be helpful. In fact bifidobacteria are much more prevalent in the gut, comprising some 90% of natural bowel flora. Many 'probiotics', as these flora supplements are known, include primarily bifidobacteria. Look for those that provide human-strain acidophilus; logically these are more likely to establish themselves in the human colon.
Conclusion
Finally, the question that most patients want to ask: is it possible to eradicate this problem permanently? The answer is yes. If you have been correctly diagnosed in the first instance, and have adhered to your prescribed diet regime, there is no reason in most cases why there should not be a successful outcome. However, there is nothing to stop it coming back. For this reason we recommend that our patients remain cautious of mould foods and excess sugar in their diets. Times when a recurrence is especially likely are during or after stressful episodes, such as allergy reactions, or infections.
References
1. Truss CO. Tissue injury induced by C. albicans: mental and neurological manifestations. J Orthomolecular Psychiatry. 7: 17-37. 1980.
2. Crook W. The Yeast Connection. Professional Books. Jackson. Tennessee. 1983.
3. Eaton KK, Howard M and McLaren Howard J. Gut permeability measured by polyethylene glycol absorption in abnormal gut fermentation as compared with food intolerance. J Roy Soc Med. 88: 63-6. 1995.
4. Eaton KK. World out of balance: the microbial-pollution connection. Wake-up call. 31st annual meeting. Amer Acad Environ Med (abstracts). 45-73. 1996.
5. Jackson PG, Lessof MH, Baker RWR et al. Intestinal permeability in patients with eczema and food allergy. Lancet. 1: 1285-6. 1981.
6. Eaton KK, McLaren Howard J, Hunnisett A et al. Abnormal gut fermentation: laboratory studies reveal deficiency of B vitamins, zinc and magnesium. J Nutr Biochem. 4: 157-63. 1994.
7. Hamilton-Miller JMT, Shah S and Smith CT. Probiotics remedies are not what they seem. Brit Med J. 312: 55-6. 1996.
Comments:
-
No Article Comments available