Positive Health Online
Your Country

History
Hayfever was first described by a physician at the beginning of the industrial revolution in 1819, who described it in himself.[1] He called it seasonal catarrh (catarrhus aestivus). It took him nearly ten years to identify a dozen other sufferers. That is how uncommon it was before the industrial revolution. Now it is twice as common in towns as it is in the country, largely as a result of road traffic pollution and the effect of sunlight on it – “petrochemical smog”.
Provocation/Neutralisation Testing.
Chronic rhinitis is estimated to affect 1 person in 6;[2] approximately three quarters of the children aged under 16 years with rhinitis, and one third of adults have allergic rhinitis with seasonal symptoms or other factors like animal exposure which can provoke the rhinitis. Itching of the nose suggests allergy. Non-infectious, non-allergic rhinitis can be diagnosed by exclusion, and usually there are food allergic components in that condition. Some people have rhinitis provoked by oral contraceptives, aspirin, pain-killing drugs which are non-steroidal anti-inflammatory drugs or by the dye tartrazine, which is used as a food colouring. Sometimes people with chronic rhinitis which is exacerbated in the summer months can have an infective cause underlying the problem. Hayfever itself, however, occurs predominantly in the grass pollen season.
The grass hayfever season usually starts around the first week in May. The hayfever season will play havoc with about 1 in 5 school children sitting important exams in May and June. The symptoms of running eyes and nose make good concentration and exam performance very difficult.
Chemical sensitivity which precedes the pollen trigger is increasingly being recognised and can also be treated.[3]
Pollution: This is largely as a result of pollution and the photochemical reaction caused by sunlight, which releases ozone from sulphur and nitrogen dioxides. Ozone is a potent sensitiser of the nasal and lung linings and makes them more likely to react allergically to pollen and dust, producing the symptoms of hayfever (itchy, runny, blocked nose and sneezing, itchy, red, streaming eyes) or of asthma (cough, wheeze and shortness of breath).
Nitrogen oxide, released from vehicle exhausts, can damage the sensitive lining of the nose at levels of 0.4 to 2.0 parts per million making sufferers more vulnerable to attack.
Particles in diesel engine fumes can enhance pollen sensitivity and produce allergic reactions in their own right. In twenty years the number of people treated for hayfever has risen by over 400% although city pollen counts have dropped. Asthma and eczema are also rising in incidence, by about 5% per year. Nitrogen dioxide levels in central London rose by 40% between 1979 and 1989.
Recent research shows that urban air may contain up to 100,000 nanometre sized particles per ml. These particles are coated with chemicals, such as ammonium sulphate derived from fossil fuel combustion, and these chemicals are irritants to the membranes of the nose, eyes, throat and lungs.
Weather: Many people suffer in sunny, bright weather as a result of the photochemical effect described above. A proportion of people, however, suffer more at the onset of wet, rainy weather and researchers in Australia have discovered that starch granules packed tightly within pollen grains are released on contact with water and these are sufficient to provoke allergic reactions in susceptible people. In the presence of rain water and high humidity each pollen grain bursts releasing about 700 granules of starch. These are each approximately 1 millionth of a metre across and can easily penetrate the airways causing asthma and hayfever.
Some people are affected more as a result of the dramatic increase of mould spores which occurs during rain and thunder storms. Patients may be more susceptible to moulds and dust during the hayfever season although they are able to tolerate them normally when they are not reacting to pollen.
Hayfever can occur at any time between February and September depending on which pollen(s) are responsible. The commonest problem is with grass and these pollens are produced from April through September.
Treatment
Traditionally treatment has involved the use of antihistamines, steroids and decongestants.Antihistamines – These drugs are often prescribed despite their frequent side-effect of drowsiness and their limited efficacy. Newer antihistamines may be less sedative but rarely do more than modify the symptoms.[4]
Steroids – These occur in different forms, injections, tablets and nasal sprays. The list of unwanted effects, including nose-bleeds, diabetes and reduced immunity to infection, is enormous and it is a measure of the distressing nature of hayfever symptoms that their use is even countenanced by doctors.
Decongestants – These are drugs which cause the lining of the nose to shrink, thus reducing the congestion which occurs as a result of histamine release in hayfever. Decongestant sprays may make matters worse as they often need to be taken with increasing frequency, in increasing dosage to achieve the same effect – indeed congestion may be worse as the effects wear off than before the product was used.[5]
Desensitisation: Since 1911 when two researchers Noon and Noon published an article in the Lancet describing the effect that low-doses of the same item as the person is sensitive to could protect against reactions from that substance, a programme called desensitisation had been employed. In this country the doses used were increasing doses and it became unfashionable medically to use this because the increasing doses could provoke reactions. However, Dr Varney et al. published a paper in the British Medical Journal[6] in which they described the usefulness of immunotherapy which is hyposensitisation in patients with severe summer hayfever. They found that their assessment confirmed there was a very significant decrease in these patients’ symptoms. A further study[7] in which people who have allergic rhinitis due to house dust mite were treated with low-dose sublingual treatment with a house dust mite vaccine to protect them against their sensitivities, showed its effectiveness. In a similar way low-dose therapy for patients with allergic rhinitis due to grass pollens has been very effective and safe. The technique of low-dose desensitisation has been debated for many years but is well established by practical application and is extremely effective for the majority of patients with hayfever.
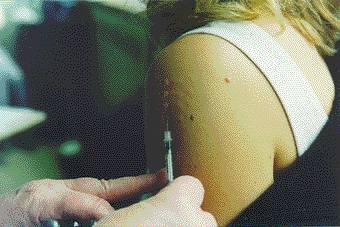
Provocation/Neutralisation: There is another treatment in the form of neutralisation. The method, called provocation/neutralisation was first described in the 1960s by an American doctor, Dr. J.B. Miller. The testing begins with a skin test of a solution of pollens which is assessed after 10 minutes. A series of weaker solutions may be tested. The aim of testing is to find the degree of sensitivity. The ultimate goal is to reach a “neutralising” dose which stops the symptoms. A neutralising cocktail is a mixture of all the neutralising points placed together in a solution and is usually taken sublingually three times a day during the hayfever season.[8,9]
These vaccines have an 80% chance of working well and have no deleterious effects on the mind or the ability to think.
Self Help: Hayfever sufferers can help themselves in a number of ways. Staying indoors with windows closed, avoiding fields, grass, cut grass and wearing sunglasses may all reduce symptoms. Avoiding pollution from traffic or industry and avoiding processed foods and wheat (closely related to grass) in the diet may also help.
|
Self help for hayfever
Outside: 1) Keep car windows and air intake closed. If air conditioned use internal circulation setting. 2) Avoid gardens, fields, picnics, barbecues, cut grass, etc. 3) Avoid city centres and areas of high traffic density as far as possible. 4) Wear good dark glasses – prevents pollen entering the eyes and protects from U.V. irritation. Inside: 1) Keep flowers outside (cut, pot, & dried). 2) Keep house dust-free (esp. bedroom). – damp dust daily – use a good vacuum cleaner with a filter daily (eg Medivac) and clean bedding, carpets, curtains and soft furnishing. – use air filters (eg Filtaire) to filter particles and chemicals from the air. – Change from feather cushions, pillows, and duvets to a washable substance such as kapok or polyester and wash all bedding (inc. pillows) once a week. – Cover duvet, pillows and mattress with a dust-mite proof fabric (eg Slumberland, Intervent, Medibed) 3) Keep windows closed. 4) Avoid chemicals, including scents, scented cosmetics and cleaning products, paint, solvents, glue, cigarette smoke, (anything that smells is emitting a chemical substance). These can make eyes, nose and throat more sensitive to dust and pollen. 5) Try to sleep in a cool bedroom, with the head propped up. 6) Ban pets from the bedroom, and avoid stroking and handling animals. 7) Take a good multimineral and multivitamin preparation (avoid vitamin A if you are pregnant). 8) Take a vitamin “C” supplement daily. 9) Take a zinc supplement each day. 10) Homoeopathic treatment has been shown to work (Dr Reilly 1986) in some hayfever sufferers. 11) Some foods can exacerbate symptoms during the hayfever season; some people are helped by avoiding wheat in the diet, others find that cutting down on histamine-containing and histamine-releasing foods is helpful (eg. cheese, strawberries, shellfish, tinned fish, pork). 12) Don’t smoke – cigarette smoke is an effective irritant which makes symptoms worse. 13) Alcohol will usually worsen symptoms. 14) Avoid decongestant sprays as they cause a “rebound” effect – symptoms are made even worse as the drug’s effect wears off. 15) If using a treatment for house dust mites use “Banamite” which is non-toxic. 16) Provocation / neutralisation. |
References:
1 Finn, R. John Bostock, hayfever, and the mechanism of allergy. The Lancet. Vol 340: Dec 12, 1992, pg 1453–1454.2 Mygind N, Weeke B (eds). Allergic and vasomotor rhinitis: clinical aspects. Copenhagen: Munksgaard, 1985.
3 Rea, W J. Chemical Sensitivity. Chelsea, MI: Lewis, Vol. 1, 1992.
4 Scadding, G K. Chronic non-infectious, non-allergic rhinitis. Prescriber’s Journal. Vol 36: No 2.
5 Scadding G K. Rhinitis medicamentosa. Clin Exp Allergy 1995; 25: 391–4.
6 Varney, V A et al. Usefulness of immunotherapy in patients with severe summer hayfever uncontrolled by antiallergic drugs. BMJ. Vol 302: 2 February 1991; 265–269.
7 Scadding G K and Brostoff J. Low dose sublingual therapy in patients with allergic rhinitis due to house dust mite.
8 Boris M, et al. Antigen induced asthma attenuated by neutralisation therapy. Clin Ecol 1985; 3: 59–62.
9 Gerrard J W, King D S. A double blind study on the value of low-dose immunotherapy in the treatment of asthma and allergic rhinitis. Clin Ecol 1989; 6: 43–6.
Comments:
-
No Article Comments available