Positive Health Online
Your Country

Photodynamic Therapy for Cancer
listed in cancer, originally published in issue 117 - November 2005
Light – absolutely required by the body, in the production of vitamin D, for example. And its lack, i.e. sunlight, can even lead to depression in a syndrome called SAD (Seasonal Affect Disorder).
Today, we use many types and forms of light in treating illness and disease, including ultraviolet, infrared and the highly concentrated light of the laser.
Ancient civilizations also practised different forms of phototherapy (treatment with light). Hippocrates recommended the use of sunbaths in ancient Greece, while in the 20th century Switzerland, Bernhard and Rollier called it heliotherapy and used it in the treatment of tuberculosis.
Given the long history of treating with light, it should come as no surprise that an effective method of battling cancer with light has been discovered. Cancer, the second greatest disease killer of mankind, can affect almost every part of the human body. For this reason, different kinds of treatment have been developed in conventional medicine, including surgery, radiation, chemotherapy and hormone therapy. Alternative medicine has its treatment modalities too, including herbs, diet and nutrition, bioelectromagnetic treatments and a host more.
But, PhotoDynamic Therapy, or PDT, offers a unique solution to those suffering from cancer, mainly because it does not require hospitalization, surgery, chemotherapy, radiation or immunotherapy. It can be used routinely and repeatedly as it selectively destroys only affected cancerous cells, thus proving it to be one of the most effective, and safest, forms of treatment.
Discovery and Applications of PDT
In 1900, a medical student named Oscar Raab, while working in a pharmaceutical laboratory, observed the effect of minute concentrations of acridine, a hydrocarbon dye, on single-celled animals called paramecia. He noticed that, somehow, daylight was affecting the results, and upon more careful study, discovered that the acridine killed the paramecia only in the presence of light, while acridine alone, and light in the absence of the acridine, did not. Light served to activate the dye! In fact, in 1903, a Nobel Prize was awarded to Niels Finsen, for his pioneering research in light treatment. It is believed that the first cancer cure using PDT, of a basal cell carcinoma of the lip, occurred in Germany in 1904.
The dye became known as a photosensitizing agent, and over the years, other such photosensitizing agents were discovered. Similarly, over time, the light source used to activate the photosensitizer became that of a cold-laser. Cold lasers are distinguished from hot ones by the fact that they generate non-thermal light which does not cut or burn tissue.
Systematic clinical studies were also undertaken to determine the clinical effects of these activated photosensitizing agents. In the 1970s, a team led by Dr TJ Dougherty of the Park Institute in Buffalo, NY, in the United States, began using porphyrin compounds as the photosensitizing agents. His research ultimately led to the US Federal Drug Administration (FDA) approving PDT as a cancer treatment for a sensitizing agent known as Photofrin®. It is in use to this very day.
But, with the advent of radiation and various chemotherapies, the PDT procedure was soon forgotten! Only recently has it begun to make a comeback and the response has been encouraging.
Some of the types of cancer that are being treated by PDT in clinics in various parts of the world include Melanoma (skin cancer), Brain, Head and Neck, Esophagus, Lung, Breast, Stomach, Pancreas, Liver, Colon, Ovarian, and Prostate. Pre-cancerous lesions known as actinic keratoses are also treatable by PDT. Research is on-going to address other types of cancers as well.
The technique itself is rather straightforward. The photosensitizing agent is either injected into the patient's bloodstream, taken orally or even applied topically. In and of itself, the photosensitizer is harmless, having no effect on the body, positively or negatively.
The agent concentrates in cancer cells of all types. One reason for this is that cancer cells are more metabolically active than normal, healthy cells. Another reason is that certain physiological properties of tumor tissue cause the photosensitizing agent to be taken up and retained by them while being excreted from most healthy tissue.
Then, the mass, with its accumulated photosensitizing agent, is subjected to a dose of laser light of a specific wavelength. The light activates the photosensitive agent causing the release of a highly reactive free-radical oxygen molecule that leads to the destruction of the cancer cell (necrosis) and especially the blood vessels feeding it. Think of it as a kind of free radical 'bomb' that blows up the cancer cell from the inside. Often, the necrotized tissue just sloughs away and there is normal healing of the wound. However, function and structure of delicate non-cancerous underlying tissue is preserved.
Further, PDT can be used to treat not only superficial tumors, but, by repeated use, large tumors too. The process is called debulking, wherein the tumor is progressively reduced in size.
What's more, PDT is not contra-indicated if other therapies are concurrently utilized, i.e. chemotherapy, radiation, etc.
Finally, by using the PDT approach, potentially disfiguring results, as can occur with surgery, can be minimized if not entirely eliminated.
Traditionally, the limitations to PDT have been the photosensitizing agents, as they can have a 'spill-over' effect, thus affecting normal tissue to some degree. There is also an overall increase in sensitivity to general sunlight for a period of days to weeks.
Arrays of Photosensitizing Agents
The first generation drugs that were porphyrin-based have given way to second and even third generation drugs. Some are based on chlorin compounds such as Meta-tetra hydroxyphenyl chlorin (Foscan® and Temoporfin® which studies show to be 200 times more effective than the porphyrin Photofrin®. Mono-L-aspartyl chlorine6 has been shown to be more readily taken up by tumour tissue than normal tissue and clears the body more rapidly.
Another group of compounds showing high promise as photosensitizing agents are the phthalocyanines group, which exhibit highly selective retention in certain tumour types.
A completely different approach is to stimulate photosensitive agents already in the body instead of introducing such a photosensitizer from outside. 5-Aminolaevulinic acid (ALA) is such an agent.
Other categories of compounds being investigated include psoralens, purpurins, porphycenes, pheophorbides, verdins, phenothiazinium, cyanines and rhodamines. It's no wonder that research funding is so desperately required to determine the best and most effective photosensitizing agents.
One member of this group, psoralens, and their derivatives, have been used for over 3,000 years in the treatment of skin disorders. Sometimes, the more things change, the more they really do stay the same!
Research into new types of photosensitizing agents is on-going. Russian pharmaceutical company Radapharma has developed Radachlorin (Photostem, PhotoFlora), for example, which is a chemically treated form of Spirulina (Spirulina platensis). Research also continues in Ukraine, where Photo Dynamic Therapy has been readily embraced. Herbs like St John's Wort (Hypericum Perforatum), are of particular research interest.
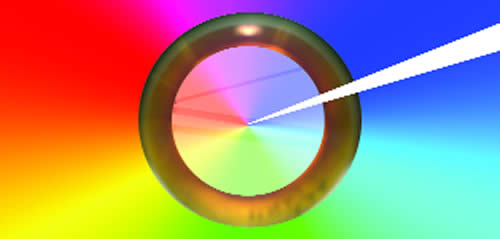
Another problem has been the inherent limitations of the laser light sources, in terms of their depth of penetration through the skin. Visible light occurs over a broad spectrum of wavelengths as shown in the following illustration:
The transmission of light through tissue is low at 400 nm because of scattering and natural absorption. Penetration of light increases with an increasing wavelength up to about 800nm, which is in the infra-red range. A specific wavelength of light is needed for each photosensitizer to maximize penetration power to the tumour tissue and to excite the photosensitizer, causing the destruction of the abnormal cell tissue.
Some of the new sensitizing agents are activated at the higher wavelengths, meaning lasers can penetrate more deeply to activate them.
The other alternative to be able to get at the malignant site and activate the sensitizing agent is by surgery, particularly endoscopic surgery and hollow needle, in order to be able to introduce the light source to the tumor. However, new laser light delivery systems are currently being developed to address even this limitation.
Side-effects of PDT
The major side-effect is photosensitivity, or sensitivity to light – a propensity to sunburn when exposed to sunlight. While inconvenient, it is hardly an 'unacceptable' risk. While previous types of photosensitizing agents remained in the body sometimes for several months, requiring the patient to stay indoors during the day (to avoid getting a severe sunburn), new agents are usually eliminated from the body after about 24 hours.
Pain is the other potential side-effect of PDT. A secondary complication, it results from the breaking down of the tumor tissue, which can cause inflammation and subsequent pain. But, it can be thought of as a 'good pain', as it indicates that the process is working! Fortunately, such pain is usually mild to moderate and easily controlled with short-acting painkillers.
Other short-term side effects may include nausea/vomiting, fever (also associated with inflammation) and occasionally, a metallic taste in the mouth. Rarely do any of these side-effects last more than a day or so.
The Leeds Centre for Photobiology and Photodynamic Therapy in England continues to do substantial research in this field, as does the National Medical Laser Centre at the University College of London (UCL). Neither limits its research efforts to PDT as it relates to just oncology (see box below).
|
PDT for Age-Related Macular Degeneration PDT is also being studied in non-oncology related illness including the treatment of atherosclerosis and both rheumatoid and inflammatory arthritis, among other diseases. But one of the most promising uses is in the treatment of Age-Related Macular Degeneration (AMD or ARMD). Results are nothing short of exceptional! ARMD affects 40% of individuals 75 years or older and is the leading cause of blindness in developed countries. One form of ARMD, the ‘wet’ form, is the result of new blood vessels formation. Termed ‘choroidal neovascularisation’ (CNV), these vessels grow under the centre of the retina, in an area known as the MACULA. There, these vessels can leak fluid and bleed, causing scar tissue to form. That scarring can destroy vision in AS LITTLE AS THREE MONTHS! In ARMD, the photosensitizing agent is also injected into the patient’s bloodstream. The light sensitive dye sticks to the inner lining of the new vessels. Then, the macula of the patient’s eye is subjected to the dose of light, which activates the photosensitive agent resulting in damage to the blood vessels, causing them to close, preventing the leaking vessels from doing further damage. The procedure is done on an out-patient basis and takes about 30 minutes. A study for the treatment of Age-Related Macular Degeneration with Photodynamic Therapy was performed in 22 centres in Europe and the United States. Vision was stable or improved in 61% of patients treated with photodynamic therapy with virtually no side-effects! |
As such research continues, the application of light as a treatment modality will only expand and will provide a safe and effective means of treating a large variety of diseases.
Because PDT so nominally impacts the body and has so few side-effects while still having a major killing effect on cancer cells, it should be considered a front-line, first choice treatment option. After all, its effects are known within days. If it proves unsuccessful there is still the traditional radiation, surgery and chemotherapy options available. But if it DOES prove effective, the patient is left without all the side-effects associated with those other treatment options.
And, of course, it may the 'treatment of last resort' when chemo and radiation therapies are ineffective and the tumour is inoperable. There really is nothing to lose and quite literally everything to gain.
There is also the consideration of PDT in terms of the cost of healthcare. Photodynamic therapy is out-patient based, often effective in one treatment, does not usually require significant surgery, provides a fast application with quick evidence as to effect, thereby reducing both waiting lists and decision times regarding other or additional treatment options. In these times of needing to find ways for cancer treatments to be affordable, can PDT option seriously be side-stepped?
Amazing, this thing we call light! So common, we usually take it for granted. But so basic that we couldn't live without it!
Additional Resources
Fedyniak LG. MD. Battling Cancer-with Light. To be published in 2006 – a consumer information book including a listing of PDT treatment centres around the world.
Henderson B et al. Photodynamic Therapy: Basic Principles and Clinical Applications. Marcel Dekker. New York. 1992
Centre for Photobiology and Photodynamic Therapy. Leeds University.
This site is especially excellent for science junkies, particularly the biochemistry of photosensitizers. www.bmb.leeds.ac.uk/pdt/index.html
The National Medical Laser Centre at the University College of London (UCL).
www.killingcancer.co.uk
National Cancer Institute (United States). Photodynamic Therapy Q & A. http://cis.nci.nih.gov/fact/7_7.htm
Oregon Medical Laser Centre. http://omlc.ogi.edu/pdt/articles/index.html
Comments:
-
Antonio-Mario Vella said..
Can you please tell me were the treatment can be taken in Russia