Positive Health Online
Your Country

Treatment Approaches to Premenstrual Syndrome
listed in women's health, originally published in issue 58 - November 2000
Since 1995, many women have sought my help for symptoms related to premenstrual syndrome (PMS). It was clear, through clinical and personal experience, that it was usual for symptoms to vary in severity and type, from woman to woman, month to month, and that lifestyle adjustments, complementary therapies and some drugs had positive effects.
Premenstrual syndromes (PMSs) are a group of menstrually-related, chronic, cyclical disorders manifested by emotional and physical symptoms in the second part of the menstrual cycle, which subside after the beginning of the menstrual period.[1]
Many doctors do not believe there is such condition as PMS and, consequently, fail to recognize and treat it. Of 482 women who called the National Association for Premenstrual Syndrome (NAPS) helpline last year, 42% said that their GPs were unsympathetic or did not seem to know much about PMS.[2]
Over the last 60 years, research has been directed towards establishing the causes and generating effective treatments for PMS. The lack of agreement about premenstrual problems as a syndrome, and its diagnosis, has contributed greatly to GPs' disbelief.
Its recognition is a twentieth-century event, reflecting changes in our social structure and lifestyle. In the past the time between puberty and the menopause was filled with many pregnancies when PMS disappears. Each was followed by the cessation of ovulation caused by prolonged breastfeeding. Nowadays, with fewer pregnancies, the effects of the menstrual cycle are more apparent.[3]
Incidence
Most women experience premenstrual symptoms during their reproductive years, but not all perceive PMS as debilitating or distressing. However, 5-10% of women – approximately 1.5 million women in the UK – suffer from such severe premenstrual symptoms (PMDD, or premenstrual dysphoric disorder) that their work, relationships and social lives are impaired. Severe PMS is more common between the ages of 30 and 40 years, and in women with young children.4 Certain hormonal events may be linked with the onset of PMS, for instance childbirth (particularly if followed by postnatal illness), cessation of oral contraception use, or sterilization. There is also evidence to suggest significant symptom exacerbation due to stress.[5]
Aetiology
The aetiology of PMS is unknown. Hormonal causes such as excessive circulating oestrogen, increased or decreased levels of progesterone, or an imbalance between oestrogen and progesterone have been proposed.[6] Other theories include:
• Aldosterone (fluid retention);
• Prolactin (direct influence on breast tissue, association with stress, and indirect relationship with dopamine and nervous pathways);
• Prostaglandin imbalance (effect of sex hormones on their synthesis).
Because PMS continues after hysterectomy if the ovaries are conserved, but disappears during pregnancy, with drug-suppressed ovulation and after the menopause when the ovaries are removed, gonadal hormones seem to be causal.[7] However, no significant hormonal differences between those with PMS and those without the disorder have been found.[8]
The current consensus is that PMS is the result of reaction to normal hormonal, biological and environmental change in susceptible women. The pathogenesis is said to involve altered central neuroregulation and disordered homeostasis. This viewpoint has encouraged the investigation of neuro-endocrine modulated central neurotransmitters and the role of the hypothalamic-pituitary-gonadal axis in PMDD.[9],[10]
Diagnosis
The absence of specific tests and inconsistent acknowledgement of over 150 symptoms contribute to the difficulty in diagnosis, which relies on charting the timing of symptoms and menstruation. Symptoms arise during the luteal phase of the menstrual cycle. If behavioural symptoms persist throughout the menstrual cycle then the disorder might be psychological or psychiatric.[11],[12]
|
Symptoms
|
|
| Psychological and behavioural symptoms
Mood swings and depression |
Physical symptoms
. |
Treatment Approaches
While the literature contains many rational arguments and trials for treatment, only three recent studies [13],[14],[15] explored women's perception of their effectiveness. None was in the UK. However, it was clear from personal clinical experience that women had a lot to say on the subject. Therefore, questionnaires were sent to members of the National Association for Premenstrual Syndrome (NAPS) in England, to find out women's assessment of the treatments they had tried.
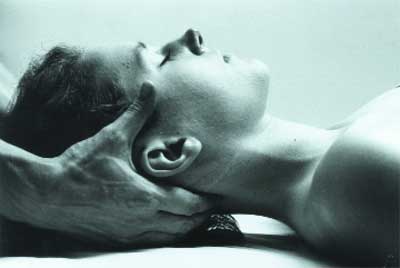
Osteopathy may help to restore normal physiological function to reproductive organs
Conventional Treatments
Progesterone:
Between the 1950s and 1980s progesterone deficiency was thought to underlie PMS and was a popular therapy. The consensus in the literature to date suggests there is no direct evidence to support this aetiology, nor its use as a treatment, although 4 out of 12 trials showed some benefit. Side effects included alteration in length of menstrual cycle.[16]
Progestogen (synthetic progesterone-like drugs):
Seven reviewed randomized controlled trials (RCTs) in 1999 found three of these reported significant improvements with the drug, and the remaining four showed no therapeutic benefit. Paradoxically, progestogens have been shown to induce PMS symptoms.[16]
Combined oral contraceptives:
Oral contraceptives (OCs) continue to be widely used to suppress ovulation; despite this only four RCTs have investigated their effectiveness. Limited evidence suggests some women may find OCs effective for some physical symptoms; however for others they intensify mood symptoms. Daily progestogen may produce PMS-like side effects and a seven-day break may allow symptom relapse, in addition to a higher risk of thromboembolic disorder in susceptible individuals. This is also true for oestrogen, danazol and GnRH analogues.[16]
Oestrogen patches/implants:
Ablates (stops) the menstrual cycle. In addition, progesterone or progestogen is needed to prevent endometrial hyperplasia in non-hysterectomized women. Side effects include breast pain, nausea and weight gain, and skin patches may irritate the skin.[5]
Bromocriptine:
Inhibits the release of prolactin; used for treating breast tenderness or mastalgia (pain). Not widely prescribed. Side effects include nausea, constipation, headache and dizziness.[17]
Danazol:
A synthetic androgen used for the relief of mastalgia (breast pain). It suppresses ovulation, but long-term cardiovascular consequences and masculinization outweigh the benefits.[16]
GnRH analogues:
Another drug that suppresses ovulation, found to have benefits. However, the maximum treatment period is six months, and hormone replacement therapy has to be given to prevent symptoms commonly seen in the menopause, including bone loss.[18]
Diuretics (e.g. Spironolactone):
Usually used for weight gain, which includes water retention. Long-term use not recommended. Side effects include potassium depletion (not Spironolactone).[16],[19]
Selective Serotonin Re-uptake Inhibitors (SSRIs):
Used for psychological and behavioural symptoms. Fourteen RCTs showed improvements compared with a placebo. Side effects include nausea, vomiting, diarrhoea, dry mouth, anxiety, headache, palpitations, dizziness and reduction in libido. Research is presently focussing on using low doses in the luteal phase to reduce side effects.[10],[16]
Mefenamic acid (non-steroidal anti-inflammatory drugs):
Current consensus in the literature suggests it is of benefit in somatic symptoms – headache and general aches and pains but not for breast pain. Side effects include gastrointestinal problems.[16],[20]
Lifestyle Treatments
Frequent intake of carbohydrates:
Tryptophan levels in the brain are associated with serotonin synthesis. Carbohydrates are said to raise these levels with a positive effect on mood and cognition. Some women with PMS eat more carbohydrate during the luteal phase, which may be an attempt at self-regulation of mood changes.21 Other research has shown no differences between glucose levels in PMS and control subjects.[7]
Caffeine and fluid intake:
A strong concordance between consumption of caffeine beverages and PMS symptoms has been found.[22] However, the evidence from the limited number of RCTs does not convincingly support advice to reduce caffeine intake and increase fluid intake.
Alcohol:
Promotes a distinct fall in plasma glucose. One study found women with PMS more likely to consume more alcohol in the symptom-free period of the menstrual cycle,22 which is in direct opposition to an earlier study which proposed that increased consumption of alcohol was a self-medicated attempt to alleviate PMS symptoms.23 However, the limited research in this area has focused mainly on alcoholic women.[24]
Sugary foods:
Stimulate insulin release, but differences in glucose levels between PMS patients and control subjects have not been found; although it has been reported that increased consumption of sugar, dairy and refined carbohydrates has been observed in PMS patients.[25] Another study found that chocolate, beer and fruit juice had a strong association with more severe PMS.[22]
Pyridoxine (Vitamin B6):
Vitamin B6 may affect the liver clearance of oestrogen, thereby relieving premenstrual symptoms, and is widely used. Conclusions drawn from an extensive review were that B6 was more effective than a placebo in relieving overall PMS symptoms and in depression associated with PMS, but it was not dose dependent. There is no evidence to suggest that women with PMS have a lower vitamin B6 status than do others.[26]
Magnesium (Mg):
Different groups have reported lowered magnesium levels in the blood cells of women affected by PMS.[27],[28] Dairy products and sugar, which are taken excessively by some PMS patients, have been shown to interfere with magnesium absorption and excretion.[25] However, the different doses used in trials and inadequate information about absorption rates in humans, make definitive interpretation of results difficult.
Zinc:
While studies have indicated lower zinc levels in PMS patients,28 none have measured its effectiveness as a treatment for the symptoms.
Calcium:
Has also been postulated to be the root of the pathophysiological changes in PMS. A rigorous, well-designed study of 441 patients found that 55% of women given calcium had a 50% global symptom improvement and suggests that calcium may affect the monoamine metabolism, reversing serotonin dysregulation. However, another study did not reveal any significant differences in the concentration of calcium in PMS and control subjects.[7]
Evening primrose oil (EPO):
Women with PMS may have a deficiency of gamma-linoleic acid (GLA) (found in EPO), a precursor of prostaglandin E1 which may lead to sensitivity to luteal phase prolactin and steroids.29 GLA has been used in combination with vitamin B6 (100-150mg per day) for premenstrual symptoms, including breast pain.30 A recent meta-analysis of clinical trials, in which only 5 were randomized placebo controlled, showed that better quality research is required.[31]
Exercise:
Although a clear physiological explanation is lacking, three RCTs have found that moderate aerobic exercise reduces negative mood states and pain.[16],[32] Hence there is more agreement here but there are methodological problems with the studies.
Relaxation: Stress may exacerbate PMS. One RCT found a 58% improvement in the relaxation response group in 46 women with PMS.[33] However, another study found no overall benefit.34 Further research is needed.

Massage may help in the treatment for anxiety, pain and water retention
Complementary and Alternative Treatments
Chiropractic:
Proposes that spinal misalignment can produce neurological interference, which can affect the health of the innervated part e.g. reproductive structures. One case study reported a universal decrease in PMS symptoms, but is not as reliable as a trial.[35]
Acupuncture:
PMS is defined both aetiologically and pathophysiologically within Traditional Chinese Medicine (TCM), which recognizes groups of signs and symptoms as a pattern of disharmony. The basic imbalance that causes PMS according to TCM is liver qi stagnation. The liver in TCM is responsible for the smooth flow of qi (energy), and reflects the rise and fall of hormones in the endocrine system. Diet, relaxation and exercise are also said to benefit the liver and release stuck qi, hence they are included in this therapeutic model. Similarly, Chinese herbs are administered according to the energetic imbalance in TCM theory. Many different herbs may be used, and no one individual is likely to receive the same prescription.[36] Specific research measuring TCM's effectiveness in PMS is lacking.

Acupuncture and Traditional Chinese Medicine attempts to restore balance to the endocrine system
Homeopathy:
Many homeopathic remedies for PMS have been listed, but, although homeopathic physicians report success, there is little scientific evidence. One placebo-controlled double-blind study failed to demonstrate the efficacy of homeopathic remedies.[37]
Light therapy:
Melatonin concentrations may represent a vulnerability factor for depressive symptoms during the menstrual cycle and patients with PMS experience substantial seasonal patterns in mood and premenstrual symptoms. A promising preliminary study showed bright light therapy to have beneficial responses in patients with PMDD.[38]
Cognitive behavioural therapy (CBT):
Five RCTs measured its efficacy in treating premenstrual dysphoric changes. One study found it more useful for symptom relief than dydrogesterone or relaxation therapy. A later study found that cognitive therapy and information regarding diet, rest and exercise given to the control group were equally effective. Two other RCTs reported its effectiveness, whereas one found no benefit.[16]
Massage:
A study of women's perceptions found that some types of massage therapy were the most effective self-help treatment for mood/anxiety, pain and water retention.[15] However, no RCTs have specifically investigated this area.
Osteopathy:
Treatment of PMS includes manipulation of facilitated segments, at the same level of innervation in visceral segments (reproductive organs). The normalization of musculoskeletal function is said to restore normal physiology through reflex actions.39 However, there have been no trials to assess its effectiveness in PMS.
Nutrition therapy:
Its efficacy in PMS has not been proven despite years of research into individual nutrients, and the nutritional status of PMS patients.[25] At present no specific research exists which examines the usefulness of individual nutrition schedules created by nutritionists for PMS patients.
What Treatments Did British Women Use for Their PMS and How Effective Did They Perceive Them to Be?
The study examined the questionnaire survey responses from 114 women.
|
Treatment Women tried
Rest 30 |
|
Perceived % effectiveness
93.3% |
* The five most commonly tried orthodox treatments were selective serotonin re-uptake inhibitors (SSRIs), progesterone, oral contraceptives, paracetamol and progestogen.
* The five most commonly tried lifestyle treatments were evening primrose oil (EPO), less caffeine, B6, frequent starchy food and exercise.
* The five most commonly tried non-orthodox treatments were massage, osteopathy, homeopathy, acupuncture and cognitive behaviour therapy (CBT).
The table above shows treatments perceived effective in the relief of PMS symptoms in over 60% of women who tried them.
Overall, rest, exercise and massage were preferred to prescribed medication. In addition, women who tried complementary therapies perceived them to be effective.
Where 50% of the women reported relief for a particular symptom it was recorded:
* EPO for painful tender or swollen breasts;
* Mefenamic acid or paracetamol for abdominal heaviness, discomfort or pain.
* Osteopathy and mefenamic acid for backache, joint or muscle pains, or stiffness;
* Diuretics for feeling bloated, oedema and puffiness or water retention.
* SSRIs, progestogen and acupuncture for feeling under stress/like you just can't cope;
* SSRIs, cognitive behaviour therapy and progesterone for feeling sad or depressed;
* Frequent starchy food, progestogen and a reduction of sugar for outbursts of irritability or anger.
Conclusion
PMS is probably the consequence of numerous physiological changes involving ovarian hormones, mineralocorticoids, prolactin, androgens, prostaglandins, nutritional factors, hypoglycaemia, endorphins and other central nervous system changes. As symptoms vary so much from woman to woman, it is likely that each has a different aetiology and all may be influenced by emotional factors.
The findings of this study largely confirm previous research except for greater use of SSRIs by women in this group. Despite this trend, a high proportion of these women perceived lifestyle adjustments – rest, exercise, less caffeine/ alcohol/sugar, increased fluid intake, frequent starchy food, and evening primrose oil (EPO) – plus complementary therapies – massage, acupuncture, cognitive behaviour therapy (CBT), osteopathy and light therapy – as effective.
It seems critical from these results that more RCTs are designed to isolate the effects of lifestyle adjustments and complementary therapies on PMS symptoms. This future research is important due to questions raised about the long-term use of SSRIs, such as whether efficacy is maintained, the emergence of side effects, or the re-emergence of symptoms, given the assumption that PMS is a long-term, cyclic and episodic disorder.
References
1. McPherson A and Waller D. Women's Health. Oxford University Press. 1997.
2. Sadler D. A GP's Perspective of PMS. NAPS. 31:4. Summer 2000.
3. Steiner M. Premenstrual Syndromes. Annual Review in Medicine. 48: 447-445. 1997.
4. Freeman E, Rickels K, Schweizer E and Ting T. Relationships Between Age and Symptom Severity Among Women Seeking Medical Treatment for Premenstrual Symptoms. Psychological Medicine. 25: 309-315. 1995.
5. Panay N et al. Premenstrual Syndrome – A Clinical Review. NAPS. 1-6. 1999.
6. Redei E and Freeman EW. Daily Plasma Estradiol and Progesterone Levels Over the Menstrual Cycle and Their Relationship to Premenstrual Symptoms. Psychoneuroendocrinology. 20(3): 259-267. 1995.
7. Roca CA, Schmidt et al. Implications of Endocrine Studies of Premenstrual Syndrome. Annals of Psychiatry. 26: 576-580. 1996.
8. Cerin A, Colilins A et al. Hormonal and Biochemical Profiles of Premenstrual Syndrome. Acta Obstetricia et Gyneclogica Scandinavica. 72: 337-343. 1993.
9. Rubinow DR and Schmidt PJ. The Neuroendocrinlogy of Menstrual Cycle Disorders. NY Academic Science. 26: 576-580. 1995.
10. Halbreich U and Smoller JW. Intermittent Luteal Phase Sertaline Treatment of Dysphoric Premenstrual Syndrome. Journal of Clinical Psychiatry. 58: 399-402. 1997.
11. Mortola JF. Issues in the Diagnosis and Research of Premenstrual Syndrome. Clinical Obstetrics and Gynecology. 35(3): 587-600. 1992.
12. Gehlert S and Chang C. Symptom Patterns of Premenstrual Dysphoric Disorder as Defined in the Diagnostic and Statistical Manual of Mental Disorders – IV. Journal of Women's Health. 8(1): 75-85. 1999.
13. Campbell EM, Peterkin DRN, O'Grady K and Fisher-Sanson R. Premenstrual Symptoms in General Practice Patients: Prevalence and Treatment. Journal of Reproductive Medicine. 42(10): 637-645. 1997.
14. Singh BB and Simpson RL. Incidence of Premenstrual Syndrome and Remedy Usage: A National Probability Sample Study. Alternative Therapies in Health and Medicine. 3: 75-79. 1998.
15. Pullon SR, Reinken JA and Sparrow MJ. Treatment of Premenstrual Symptoms in Wellington Women. New Zealand Medical Journal. 102: 72-4. 1989.
16. Wyatt KM, Dimmock PW and O'Brien PMS. Premenstrual Syndrome. Clinical Evidence. 1: 286-297. 1999.
17. Andersch B. Bromocriptine and Premenstrual Symptoms: A Survey of Double Blind Trials. Obstetrical and Gynecological Survey. 38(11): 643-646. 1983.
18. West CP and Hillier H. Ovarian Suppression with the Gonadotrophin-releasing Hormone Agonist Goserelin (Zoladex) in the Management of the Premenstrual Tension Syndrome. Human Reproduction. 9(6): 1058-1063. 1994.
19. Wang M, Hammarback S, Lindhe BA and Backstrom T. Treatment of Premenstrual Syndrome by Spironolactone: A Double Blind, Placebo-controlled Trial. Acta Obstetricia et Gyneclogica Scandinavica. 74: 803-808. 1995.
20. Budoff PW. Use of Prostaglandin Inhibitors in the Treatment of PMS. Clinical Obstetrics and Gynecology. 30: 453-464. 1987.
21. Christensen L. Effects of Eating Behaviour on Mood: A Review of the Literature. International Journal of Eating Disorders 14(2): 171-183. 1993.
22. Rossignol AM & Bonnlander H. Prevalence and Severity of the Premenstrual Syndrome: Effects of Food and Beverages that are Sweet or High in Sugar Content. Journal of Reproductive Medicine 36: 131-39. 1991.
23. Caan B, Duncan D et al. Association Between Alcoholic and Caffeinated Beverages and Premenstrual Syndrome. Journal of Reproductive Medicine. 38(8): 630-636. 1993.
24. Halliday A, Bush B and Cleary P. Alcohol Abuse in Women Seeking Gynecological Care. Obstetrics and Gynecology. 68: 322. 1986.
25. Goei GS. Dietary Patterns of Patients with Premenstrual Tension. Journal of Applied Nutrition. 34: 4-11. 1982.
26. Wyatt K M, Dimmock PW et al. Efficacy of Vitamin B6 in the Treatment of Premenstrual Syndrome: Systematic Review. British Medical Journal. 318: 1375-1381. 1999.
27. Rosenstein DL, Elin RJ et al. Magnesium Measures Across the Menstrual Cycle in Premenstrual Syndrome. Journal of Biological Psychiatry. 35: 557-565. 1994.
28. Posaci C, Erten O, Uren A and Acar B. Plasma Copper Zinc and Magnesium Levels in Patients with Premenstrual Tension Syndrome. Acta Obstetricia et Gyneclogica Scandinavica. 73: 452-454. 1994.
29. Horrobin DF. The Role of Essential Fatty Acids and Prostaglandins in the Premenstrual Syndrome. Journal of Reproductive Medicine. 28: 465-468. 1983.
30. Brush MG. Vitamin B6 treatment of premenstrual syndrome. Curr Topics in Nutr Dis. 19: 363-79.1988.
31. Budeiri D et al. Is evening primrose oil of value in the treatment of premenstrual syndrome? Control Clin Trials 17(1): 60-8. 1996.
32. Aganoff JA and Boyle GJ. Aerobic Exercise, Mood States and Menstrual Cycle Symptoms. Journal of Psychosomatic Research. 38: 183-192. 1994.
33. Goodale IL, Domar AD and Benson H. Alleviation of Premenstrual Syndrome Symptoms with the Relaxation Response. Obstetrics and Gynecology. 75: 649-655. 1990.
34. Kirkby RJ. Changes in Premenstrual Symptoms and Irrational Thinking Following Cognitive Behavioural Coping Skills Training. Journal of Consulting and Clinical Psychology. 62(5): 1026-1032. 1994.
35. Stude DE. The Management of Symptoms Associated with Premenstrual Syndrome. Journal of Manipulative and Physiological Therapeutics. 14(3): 209-216. 1991.
36. Deadman P. Acupuncture in the Treatment of Premenstrual Syndrome. Journal of Chinese Medicine. 48: 5-14. 1995.
37. Chapman EH, Angelica J et al. Results of the Homeopathic Treatment of PMS. Journal of The American Institute of Homoeopaths. 87(1): 14-21. 1994.
38. Anderson DJ, Legg NJ and Ridout DA. Preliminary Trial of Photic Stimulation for Premenstrual Syndrome. Journal of Obstetrics and Gynaecology. 17(1): 76-79. 1997.
39. Giovanna D, Eileen L and Schiovitz S eds. An Osteopathic Approach to Diagnosis and Treatment. 2nd ed. Lippincoh-Raven, Philadelphia. pp454-459. 1997.
Comments:
-
No Article Comments available