Positive Health Online
Your Country

Pelvic Organ Prolapse: Help and Hope
listed in women's health, originally published in issue 193 - April 2012
Pelvic organ prolapse is an extremely common female health condition that has been on medical record for over 3000 years; unfortunately it has received little acknowledgment until recently. Women in every country around the world experience symptoms of POP yet have little idea what is occurring in their bodies because they are too embarrassed to discuss it with anyone. It's long past time to shift recognition and get the dialogue established.
  |
Pelvic organ prolapse (POP) can occur when the PC or pelvic floor muscles weaken and one or more organ/tissue areas shift out of their normal positions into the vaginal canal. In advanced cases of POP tissues bulge outside of the vagina; the worst case scenario is a woman's uterus can be completely outside of her body. There are 5 types of POP; organs that can prolapse are the bladder (cystocele), intestines (enterocele), rectum (rectocele), uterus (uterine), and vagina (vaginal vault). There are 4 levels of severity; grade 1 is the mildest, grade 4 the most severe.
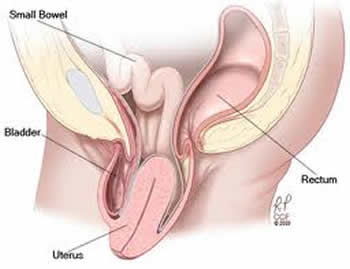
Organs that can prolapse
Statistics for prevalence of pelvic organ prolapse in most countries are sorely lacking; the true figures are difficult to estimate because there is little screening in place and many women are too embarrassed to mention symptoms to their physicians. The current estimate for numbers of cases of pelvic organ prolapse in the US is 3.3 million; there are 600,000 women in Nepal with uterine prolapse. A study by WHO (World Health Organization) indicated that half of the women in their study in Lebanon had at least 1 type of prolapse. ‘Guestimates’ indicate that there are 34 million women worldwide with POP; this condition is common in both developed and developing countries. Since vaginal childbirth and menopause are the 2 leading causes, nearly every woman has at least 1 hash mark on her risk factor profile. Women with POP typically have multiple risk factors, but even 1 damaging child birthing experience can be sufficient to cause problems with the pelvic floor that evolve into pelvic organ prolapse. Half of all women over the age of 50 suffer from at least one type of pelvic organ prolapse (there are 5 types); many women in their 20s, 30s and 40s have POP as well.
Statistics
The demographics for POP studies typically have prominent numbers of women over the age of 50 and Caucasian, rather than including young women who have given birth and a more diverse balance of women from multiple nationalities. Accurate data related to occurrence and impact of pelvic organ prolapse will be more readily attainable after pelvic organ prolapse becomes common knowledge and the stigma is reduced. Because studies related to pelvic organ prolapse are now beginning to become more widespread, statistics may shift significantly in the near future. In general, most women do not disclose indicators of pelvic organ prolapse to physicians because of embarrassment related to symptoms.
Some current statistics related to pelvic organ prolapse are:
- Research indicates that in 2010 there were 3.3 million women in the US alone with pelvic organ prolapse;
- 40-70% of women have urinary incontinence (stat varies greatly by study, not all UI is related to POP but UI is the most common symptom of POP);
- There are 300,000 surgeries annually in the US for POP;
- 1/3 of women of women with pelvic organ prolapse will have multiple POP surgeries;
- More than half of women over the age of 50 suffer from 1 or more types of POP;
- 1 out of 3 women suffer sphincter damage during childbirth resulting in faecal incontinence;
- 20% of the women in the UK waiting for major gynaecological surgery are women with pelvic organ prolapse;
- In 2010 there were 6,929,000 females in the USA who finished road races; 30-40% of women experience urinary leakage while exercising (running, jogging, aerobics).
Research related to vaginal childbirth indicates that women are predisposed to the following types of damage that lead to pelvic organ prolapse:
- Denervation of pelvic floor muscles;
- Pressure on organs/tissues;
- Pudendal nerve denervation (crush or stretch);
- Levator Ani Denervation;
- Connective tissue damage (fascia);
- Pelvic floor muscle weakening;
- Mechanical disruption of sphincter;
- Hormonal effects of pregnancy.
Symptoms
Each of the 5 types of POP has its own symptoms, but in general the most common symptoms can include:
- Pressure, pain, or ‘fullness’ in vagina or rectum or both;
- Sensation of ‘your insides falling out’;
- Urinary incontinence;
- Urine retention;
- Faecal incontinence;
- Chronic constipation;
- Back/abdominal pain;
- Can't keep a tampon in;
- Painful intercourse;
- Lack of sexual sensation;
- Leakage of urine or stool during intimacy.
Causes
There are multiple causes of POP; factors vary with age/nationality and occupation and it is likely that most women have more than one cause of significance and additional contributing factors that add to individual dynamic. The most common causes of POP are:
- Vaginal childbirth - complications from large birth weight babies, long 2nd stage labour, damage to nerves, forceps or suction deliveries, multiple childbirths, improperly repaired episiotomies. POP that occurs because of impact of childbirth may occur after a difficult delivery or may not show up until 20 years later;
- Menopause - age related muscle impact due to drop in oestrogen level; this impacts strength, elasticity, and density of muscle tissue;
- Chronic constipation - IBS (irritable bowel syndrome), poor diet, or lack of exercise can cause constipation;
- Chronic coughing - smoking, allergies, bronchitis, and emphysema can create chronic coughing;
- Heavy lifting - lifting children, repetitive heavy lifting at work, weight trainers;
- Aggressive exercise - joggers, marathon runners, aerobics-constant downward pounding of internal structures;
- Genetics - having a family member with POP means you are more likely to have POP issue;
- Neuromuscular diseases - MS, diabetic neuropathy, Marfans (collagen deficiency), or Ehlers-Danlos Syndrome (joint hypermobility and tissue fragility).
It is also possible for women who have never given birth to have POP; there are many non-childbirth related causes.
Diagnosis
The diagnosis process for pelvic organ prolapse will vary, based on type your physician suspects you have and the tests your physician is familiar with and prefers to utilize. Traditionally the basic check for POP will start with a pelvic exam. Once it is determined you have pelvic organ prolapse, additional tests that may be utilized could be:
- Digital rectal exam;
- Pelvic ultrasound;
- Pelvic MRI;
- Urodynamic study;
- Pelvic floor strength tests;
- Hormone level evaluation;
- Cystourethroscopy.
There are multiple treatment options for pelvic organ prolapse, both surgical and non-surgical. The first step is to get a definitive diagnosis of type(s) and degree of pelvic organ prolapse. Since there are multiple layers to the POP dynamic, you are most likely to have success with your treatment path of choice if you know exactly what kinds of POP need to be treated. Each treatment has unique benefits, and which choice you make will be influenced by your personal dynamic, type of POP, whether or not you are through having children, age, length of time you have been suffering with symptoms, intensity of symptoms, additional medical conditions, your desire to have a normal sex life, and financial considerations.
The physicians who are fellowship trained in pelvic organ prolapse are urogynaecologists; additionally some urologists specialize in pelvic floor conditions. There are also some gynaecologists who treat pelvic organ prolapse, but a specialist will give you greater potential for successful treatment. A fellowship trained urogynaecologist or urologist will be able to advise patients about both surgical and non-surgical treatment options.
Surgical Treatment Options
There are multiple surgical treatment options for pelvic organ prolapse; once a definitive diagnosis is in place, you surgical choices will be outlined by your physician. Surgical treatment options include a variety of choices within each category; type utilized will vary with type/degree of POP and surgeon/patient choice:
- Abdominal repair;
- Transvaginal repairs (through the vagina);
- Robotic repairs;
- Laparoscopic repairs;
- Combinations of the above.
Some physicians utilize polypropylene mesh for pelvic organ prolapse repair. There is considerable controversy regarding the use of polypropylene mesh for transvaginal procedures; some physicians refuse to utilize it in any POP repairs, others use it exclusively for abdominal procedures, and a significant number of surgeons feel it is an intricate tool for long term results. Worth noting is the fact that POP repairs that do not incorporate mesh nearly always fail in 2-5 years because stitching weakened human tissue for support typically fails in time.
Non-surgical Treatment Options
Often when women prefer non-surgical treatment, they are referred to physical therapists or physiotherapists. Pelvic floor physical therapists have a significant variety of treatment options they can offer a woman with pelvic organ prolapse; since women's needs vary considerably based on type/degree of prolapse; treatment regimens will be a bit unique from individual to individual.
There are multiple non-surgical treatment options for POP, often women will utilize two or three treatment options at the same time for the best improvement of their symptoms. Non-surgical treatment options include:
- Kegel Exercises;
- Kegel assist devices;
- Pessary;
- Incostress;
- Core strengthening exercises (pilates, Pfilates);
- Biofeedback;
- Electrical Stimulation;
- Hormone replacement therapy;
- Support garments;
- Tibial nerve stimulation.
Impact to Sexuality
One aspect of pelvic organ prolapse that is significant and gets little press is the impact this condition has to intimacy. Faecal incontinence, urine or stool leakage during intercourse, painful intercourse, or loss of sensation can have significant ramifications on an intimate relationship. Open communication between partners is ideal, but seldom occurs with the embarrassing symptoms that pelvic organ prolapse displays. Spontaneity is difficult to achieve and any of these symptoms can create a significant gap in a relationship. The norm is women are too embarrassed to disclose these symptoms to their partners, and men assume women are not engaging in intimacy because they have no interest. The impact to relationships is considerable. When a medical condition is not disclosed to intimate partners, it creates boundaries that are difficult to overcome. When women are not aware of the cause of the symptoms they are experiencing and are too embarrassed by them to disclose details to their physicians, they usually have no idea how to address them.
Help and Hope for Women
Pelvic organ prolapse is a global women's health pandemic; since vaginal childbirth and menopause are the two leading causes, nearly every woman has at least one hash mark on her risk factor profile. Pelvic organ prolapse undoubtedly encompasses the largest demographic of all women's health issues. The dynamic behind pelvic organ prolapse is likely more diverse than any other health condition women will experience. Multiple types of pelvic organ prolapse display a variety of symptoms; women's unique backdrops related to childbirth, occupation, genetics, general health, and social activities vary significantly. The demographic is difficult to narrow down into specific slots. Countless women suffer silently with symptoms that they can't make any sense out of. When we don't know what to tie symptoms to, our minds can be our worst enemies, imagining the most negative scenario.
There is hope for women with POP; treatment options evolve daily that can be utilized to control, improve, or repair this cryptic health condition. The most positive direction we can take is to increase awareness so women start recognizing POP symptoms when they first occur. Women who have been diagnosed with POP need to come out of the closet with their diagnosis and treatment paths and share that information with other women, their mothers, their daughters, their sisters, their friends. Once we take pelvic organ prolapse out of the closet and make it common knowledge for women and the health care community starts including routine screening for pelvic organ prolapse during pelvic exams, POP will become more readily identifiable and women will be able to seek earlier, less aggressive treatment.
Resources
www.urologyteam.com/pelvic-organ-prolapse-0
https://ewhu.co.uk/conditions/pelvic-organ-prolapse
www.urmc.rochester.edu/smd/gme/prospective/obgyn/documents/wk103PelvicorganprolpaseinWHI.pdf
www.who.int/bulletin/volumes/81/9/Deeb.pdf
www.americanmedicalsystems.com/DAM_public/5823.pdf
Further Information
Gaynor Morgan, the CEO of C&G Medicare, is the sitting president of APOPS Europe and addresses needs for women regarding POP and incontinence in European countries; she can be contacted at Tel: 0871 218 1233 with related questions. The book Pelvic Organ Prolapse: The Silent Epidemic can be purchased through her website at www.candgmedicare.com ; a portion of book sale proceeds are donated to APOPS.
Comments:
-
Teresa Gabel said..
This is an EXCELLENT article. I was diagnosed with uterine and cystocele prolapses recently and will need surgery to correct things. I have been all over the internet reading everything I can get my hands on. This article covers every aspect of POP and then some. Thank you!
-
Anna Wong said..
I am into my 4th week of recovering from a vaginal hysterectomy due to prolapse of the cervix