Positive Health Online
Your Country

How to use Natural Progesterone
by Dr John Lee, M.D.(more info)
listed in women's health, originally published in issue 21 - August 1997
First, we must be clear about what is meant by 'natural progesterone'. There are, of course, a large number of plants containing progesterone-like compounds just as a large number of plants contain oestrogen-like compounds. Throughout my book, I have tried to be consistent in referring to these 'natural' oestrogen-like compounds as 'oestrogenic' substances. There is no specific hormone named 'oestrogen'; oestrogen is a class name and there are 20 or so members of this class made by the human body; the major ones being oestrone, oestradiol, and oestriol. In the case of progesterone, there is but one progestational hormone made by the human body and its name is progesterone. That is what is meant by natural progesterone.
From what source does the natural progesterone used in various treatment forms come? Early in the course of progesterone research history, progesterone was obtained from sows' corpora lutea. This was expensive and of low yield. A better source is the human placenta.
The placenta is a veritable progesterone factory, making 300—400 mg per day during the last trimester of pregnancy. At child-birth, placentas can be quick-frozen and sent to a pharmaceutical firm for extraction of the progesterone they contain. Even more economical is the use of progesterone-like plant sterols, named saponins. Upon hydrolysation, saponins are converted to sapogenins, of which two (sarsasapogenin and diosgenin) are the main source for the derivation of natural progesterone for medical use. Through the wonders of modern chemistry, it is possible to synthesise progesterone from air, coal and water but starting from the ready-made sapogenins from plants is by far the more efficient and productive way to go. From them, pure U.S.P. grade progesterone can be produced inexpensively and in great quantity.
Ironically, the majority of progesterone produced is bought by other pharmaceutical firms for further synthesis to 'unnatural' progesterone-like compounds, termed progestins, for use in their patent(ed) medicines. Some progestins are synthesised from the male hormone, testosterone, such as might be obtained from horse urine, as the hormone, oestrone, is for Premarin (from pregnant mares). Figure 1 (below) depicts the molecular transformation of sapogenins.
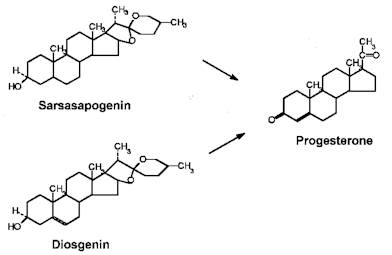
Figure 1: Derivation of progesterone from sarsasapogenin or diosgenin.
The importance of understanding this derivation of progesterone from plant saponins is two-fold. One, when fresh saponin-rich plants such as yams are eaten, our body derives progesterone-like effects from them. The July 1992 National Geographic contained a report of life on the Trobriand Islands (a small island group off S.E. New Guinea) and the people who are generally slim and happy, enjoy wonderful health (except for tuberculosis, leprosy and malaria), have a vigorous sexual life and (strangely, to the authors) fewer children than might be expected, and whose diet is dedicated to the yam, other vegetables, and fish. The yam, in fact, is a Trobriand totem signifying good health and good life. Trobriand islanders regard their life as idyllic, as do the occasional visitors. The November 1992 National Geographic contained several letters to the editor, explaining that yams contain the sterol, diosgenin, with progesterone-like effects which accounts for the Trobriander islanders' idyllic life style and lower birth rate. Progesterone, after all, is the basis for all oral contraceptives. One writer reports that 'Organon, a leading producer of contraceptive pills, uses the diosgenin from Mexican yam roots as the raw material for its products.' Yet, more than a few US physicians have no idea that their progestins are made from yams.
Second, products that list yam extract among their ingredients may or may not include the saponin-rich portion of yam root, and they may or may not include actual U.S.P. grade progesterone derived from yam (or a number of other plant sources) which is widely available. The reason for this confusion will be difficult for readers not familiar with the US to understand. The reason stems not from a deliberate deception on the part of the product producers but from our set of poorly worded laws regulating drugs as distinguished from herbs, foods, drinks, confections and condiments, apparently operating under the delusion that the biochemical effects from such-like are somehow different than those from 'drugs'. To sell 'drugs', you see, requires a license and a degree of some kind, whereas just about anybody can sell foods and herbs. As if this confusion were not bad enough, the American FDA (Federal Drug Administration) has occasional fits of overzealous interpretation of the laws and attacks purveyors of teas and vitamins and what-not with costly legal (?) suits and little comprehension of the facts of the matter. Thus the contrivance of benign labelling. Admittedly not a good thing, but I think it is helpful to understand the basis of the present confusion.
My reason for going into all this is that I am about to tell you how I use a progesterone product to treat various conditions and I am not all that familiar with all the progesterone products now on the market. I became interested in this in 1978 when I heard Professor Ray Peat, Ph.D., of Blake College, Eugene, Oregon, talk about the various attributes of progesterone. It was from him that I learned of a certain skin cream, called 'Cielo', and sold as a skin moisturiser (and it certainly is), which contained, among its other ingredients, natural progesterone. Later, when confronted with osteoporotic patients who could not use oestrogen because of history of uterine or breast cancer, or diabetes, or vascular disorders, etc., I chose to recommend this cream, hoping it would do something for their bones. And, to my considerable surprise, it did; their bone mineral density tests showed progressive improvement! Not knowing what dose to give, I used serial BMD tests to adjust dosage so that improvement occurred. It did not matter to me what dose of progesterone was in the cream; what mattered was that (1) it was safe to use, and (2) the right dose is the one that works.
Over the years since then, other companies have developed other products containing progesterone or yam extract or other extract purported to include progesterone. From following the literature, I know that Dr Joel T. Hargrove, of Vanderbilt University Medical Centre, uses progesterone in capsule form; and Dr Katherine Dalton, of London, England, uses progesterone in rectal suppositories. I used transdermal progesterone cream because I found it works, was inexpensive, and was acceptable by the patients. The transdermal route appealed to me because it avoided the first-pass loss through the liver. The original 'Cielo' is now marketed as 'Pro-Gest' cream and, for what it's worth, I am given to understand that a 2-oz jar of it contains approximately 960 mg of progesterone. If that information helps anyone, they are welcome to it. Because of the excellent results in my patients, I have stuck to that delivery system and therefore know little of the other products on the market. The company, Professional and Technical Services, Inc., of Portland, Oregon, also markets a Pro-Gest liquid, with three times the concentration of progesterone as found in their Pro-Gest cream, designed for use as sublingual drops. Since absorption through mucosa is more rapid and and more efficient than through the dermis, I would suspect that its progesterone effects are more rapid than the cream. Most of my patients through the years are content to use the cream, especially because of its obvious benefit to skin where applied.
Progesterone treatment recommendations:
General considerations
A. Transdermal absorption
It is well known that all the gonadal hormones, being small, fat-soluble molecules, are well absorbed through the skin; better, in fact, than when given orally. Oestradiol, for instance, given as a trans-dermal patch containing 0.05 mg applied twice weekly is equivalent to oral doses of 1 mg daily. That is, 0.1 mg transdermally = 7 mg orally, or 70 times more efficient, the difference being the first-pass loss through the liver of oral doses. Similar efficiency occurs with testosterone and progesterone.
B. Distribution throughout the body
In applying progesterone-containing cream, I recommend using the largest possible areas of relatively thin skin, rotating among various skin sites daily for maximum absorption. Skin sites recommended are the inner aspects of the arms and thighs, the face and neck, the upper chest and the abdomen. In dermal transport, progesterone is first absorbed into the subcutaneous fat layer and then passively diffused throughout the body via blood circulation. Initially, in progesterone-deficient patients, much of the progesterone is absorbed into body fat. With continued use, fat levels of progesterone reach an equilibrium such that successive doses of progesterone result in increased blood levels and stronger physiological effects. Thus, it is wise to tell women that progesterone applications may require two to three months of use before maximum benefits are experienced.
When produced by the corpus luteum, progesterone is embedded in a protein envelope, cortisol binding globulin (CBG), for solubility in plasma, with only 2—10% of progesterone in the free (unbound) state. Similarly, oestrogen is embedded in sex hormone binding globulin (SHBG) for transport in plasma and cholesterol is circulated enveloped in various lipo-proteins. It is not presently known whether progesterone absorbed transdermally or orally acquires a CBG carrier envelope or whether it binds temporarily to fat soluble components of cell membranes (such as, of red blood cells) for transport through blood circulation. Thus, plasma progesterone levels may not accurately measure the total progesterone available. Dosage adequacy is determined ultimately by the effects produced. (See 'Progesterone dosage' below.)
In postmenopausal women concomitantly using oestrogen supplements, the initial effect of progesterone is to sensitise oestrogen receptors, leading to heightened oestrogen effects such as breast swelling and tenderness, fluid retention, or even the appearance of scant vaginal bleeding. Therefore, I generally advise such women to reduce their oestrogen dose by one-half when starting on progesterone.
Later, after 3—4 months of progesterone use, many women can reduce their oestrogen dose further or eventually discontinue it, using adequacy of vaginal secretions as their guide.
During the perimenopausal phase, when women are experiencing changing patterns of menstruation, including missed menses, the addition of natural progesterone may temporarily bring a return to normal monthly menses. This temporary heightened sensitivity of oestrogen receptors may lead the woman (and her doctor) to conclude that progesterone caused the menses, whereas, in fact, the normal oestrogen caused the endometrial proliferation and the quitting of the progesterone each month (see 'Dosage cycling' below), allowed the shedding of whatever proliferative endometrium had developed. This is a normal state of affairs and not a cause for alarm.
C. Dosage cycling
Continued exposure of hormone signals (or other receptor signals such as sound or light) leads eventually to reduced receptor sensitivity. Our receptors 'tune down' their sensitivity to prolonged exposure by the receptor stimulator. This is obvious in the case of sound or light. A sufficient period of quiet will bring about renewed sensitivity to sound just as a period of darkness will allow increased sensitivity to dim light, so-called 'dark adaptation'. The same is true of transdermal nitroglycerin, for instance. If nitroglycerine patches or ointment are used continuously, its effect on coronary artery relaxation will diminish; occasional periods of non-use will restore its effectiveness. And the same is true of the hormones. Recall that, during regular monthly menstruation, there occurs a week or so each month of low hormone levels.
Thus, I recommend that progesterone be cycled monthly. In post-menopausal women, progesterone may be used 2—3 weeks of the month and then discontinued until the next month. A period of at least 5—7 days should be hormone free. In perimenopausal patients, I recommend timing the progesterone use to approximate normal corpus luteal production of progesterone, i.e. from day 12 to day 26 of the menstrual cycle. On occasion, this may be difficult to do with precision if menses are occurring irregularly. If, after using progesterone for a week or so and some spotting occurs, I usually recommend that the progesterone be halted for 12 days and then started anew.
D. Progesterone dosage
Though it is known that normal corpus luteum progesterone production may reach 20—-25 mg per day, it is also true that wide individual variability is the rule. The same is probably also true of one's efficiency in transdermal absorption. Further, since oestrogen and progesterone have many mutual antagonistic effects, prevailing oestrogen levels will affect the results of a given dose of progesterone. Third, the progesterone dose must be related to the effect one wishes to promote. In PMS, the dose must be high to counter the effects of prevailing, previously unopposed, oestrogen. The dose is determined essentially by trial and error. The same is true in the perimenopausal state. After menopause, when oestrogen levels are low and the desired effect is new bone formation, effective progesterone doses may be considerably lower than those needed for PMS. In treating postmenopausal osteoporosis, serial BMD testing can be used to determine progesterone dose. Thus, clinical judgment by both the patient and her doctor is desirable for the most effective use of supplemental natural progesterone. Because of the great safety of natural progesterone, considerable latitude is allowed.
E. When a woman is also on a progestin
When a woman on progestins wishes to switch to natural progesterone, several considerations should be kept in mind. First, both compete for receptor sites. The benefits of natural progesterone will be reduced by the presence of the progestin. Second, plasma progesterone levels will not reach maximum levels until the 2nd or 3rd month of use, as described in B above. Therefore, I usually recommend gradual decrease of progestin dose, such as reducing to ½ of previous dose when starting natural progesterone. During the second month of progesterone, the progestin dose can be reduced further (such as taking the reduced dose every other day). By the third month, the progestin can be safely discontinued.
Extracted from Natural Progesterone: The multiple roles of a remarkable hormone, by Dr John Lee. Published by Jon Carpenter Publishing, Unit 2PH, The Spendlove Centre, Charlbury OX7 3PQ, price £9.99, postage free. The book includes information on obtaining natural progesterone.
Comments:
-
Valerie said..
Is it wrong to use natural progesterone with a Mirena implanted?