Positive Health Online
Your Country

A Vaccine may be Here - But Where Now for Vitamin D and Covid 19 Research?
listed in infections and inflammation, originally published in issue 270 - May 2021
With the arrival of multiple Covid 19 vaccines, it is worthwhile speculating the fate of research into the effects that vitamin D might have on the virus, not just in terms of it contributing to overall immunity and any influence on morbidity and mortality, but beyond this short-term fascination.
It is easy to forget, it was only in April of last year that the UK government updated its advice on vitamin D supplementation to protect bone and muscle health, urging everyone to take a daily 10 μg supplement to mitigate the effects of reduced time outdoors as a consequence of lockdown. The benefits of supplements were further emphasised for people from black and minority ethnic backgrounds, who may not get enough vitamin D from sunlight.
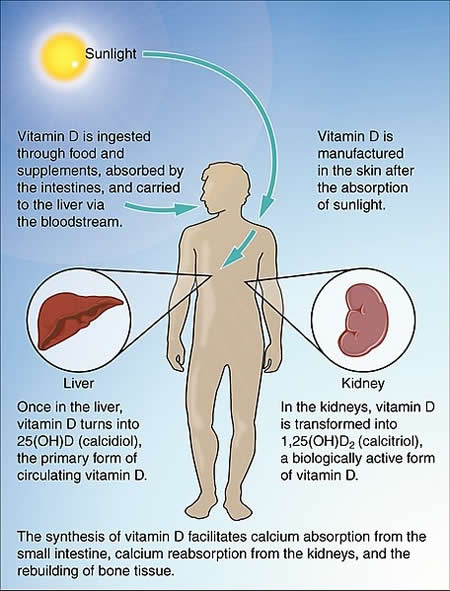
Synthesis of Vitamin D Courtesy Wikipedia
Vitamin D Deficiency And Covid 19 – Untangling The Mounting Evidence Around Two Colliding Pandemics
However, in the wake of this advice, two rapid reviews by public health agencies in England concluded there was insufficient evidence to determine whether vitamin D supplementation could have a role in reducing the risk of respiratory tract infections, including covid-19. [1,2] In contrast, a third rapid review – from the Royal Society – concluded that vitamin D deficiency is associated with an increased risk of respiratory viral infections and that it is “biologically plausible” that vitamin D deficiency may contribute to susceptibility to covid-19 infection because such a deficiency is likely to cause immune dysregulation, which may reduce the first line of defence against covid-19. It called on the government to provide a stronger public message around existing recommendations for vitamin D intake, and for more research into whether vitamin D deficiency might contribute to increased covid-19 risk seen in elderly and black, Asian, and minority ethnic (BAME) groups.[3]
Added to this, since then there have been a significant number of studies from around the world examining the possible association between vitamin D status and susceptibility to Covid 19 and its consequences. Many are retrospective cohort analyses, and some are prospective studies involving sufficiently different patient populations, with different degrees of severity of symptoms and prognoses, and indeed varying definitions of the state of vitamin D sufficiency to make meaningful systematic review/s and/or meta-analysis difficult. Nevertheless, with a few exceptions in the 50+ references appearing since April 2020 from around the world with many cited hereafter, it does appear that a higher vitamin D status is generally associated with a lower susceptibility to Covid 19, and better morbidity and mortality outcomes. [4-53] However, the definitive degree of any correlation, if any, remains, at present, to be established, as does the likely efficacy of vitamin D supplementation as an intervention.
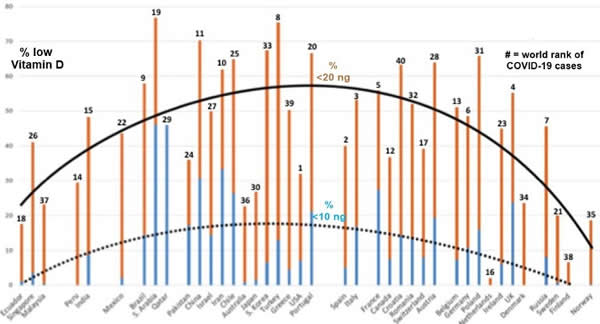
Scientific Strabismus' or Two Related Pandemics: COVID-19 & Vitamin D Deficiency. Courtesy vitamindwiki.com
Br J Nutr. 2020 May 12;1-20. doi: 10.1017/S0007114520001749. Murat Kara 1, Timur Ekiz 2 timurekiz@gmail.com , Vincenzo Ricci 3, Özgür Kara 4, Ke-Vin Chang, Levent Özçakar 1
Has this been another winter of D-iscontent
However, whilst, experts and consumers strive to establish the validity of the conflicting reviews on vitamin D and Covid 19, it is important not to forget that still today almost one in five adults aged 19–65 years in the UK has a low serum vitamin D concentration (below 25 nmol/l-considered sufficiency by SACN) according to the National Diet and Nutrition Survey (NDNS),[54] which puts them at increased risk of the manifestations of vitamin D deficiency and a wide range of health outcomes such as rickets, osteomalacia and falls, and denied benefits for muscle strength and muscle function in adults ≥50 years.
And, as winter starts to recede, it is worth remembering SACN reported that on average. [55,56] around 30–40% had concentrations below 25 nmol/l in winter compared to 2–13% in summer but a substantial percentage of some population groups did not achieve a plasma concentration ≥25 nmol/l even in summer (17% adults in Scotland, 16% adults in London, 53% of women of South Asian origin living in the south of England and 29% of pregnant women in a study in North West London).
There are many possible explanations for this state of affairs, but one is apparent in a UK study which identified specific knowledge of dietary sources of vitamin D to be poor; oily fish, considered the best dietary source of vitamin D, was only identified by half the population .[57] A considerable proportion incorrectly reported dairy products and vegetables as sources, a mistake also reported by other studies. Interestingly red meat, which according to the NDNS (2014) UK report is the largest contributor to vitamin D intake across age groups, was reported as a source by a minority. Vitamin D is naturally present in foods in limited amounts and while the majority of the population felt dietary sources were not sufficient to maintain 25-OH-D concentration, almost a third of participants believed they were sufficient or were uncertain. Hence, if individuals are unaware of the minimal dietary sources of vitamin D and also do not take supplements, vitamin D status will undoubtedly likely to be poor during winter. Furthermore, a lack of awareness was observed regarding SACN (2016) vitamin D recommendations of 10 µg supplementation, while only 69% of those who reported awareness, chose the correct RNI. Considering the difficulty in achieving vitamin D sufficiency, individuals are unlikely to achieve recommendations if they are unaware of them.
Still a Role for Vitamin D in the Wake of the Vaccine?
So, with the availability of several Covid 19 vaccines does this mean that attention might be focussed away from concern about the high levels of vitamin D deficiency that appear to adversely compromise health and increase susceptibility to the virus? This need not be so for a number of reasons. The most important reason to recommend otherwise, is the role well recognised vitamin D has in supporting both innate and adaptive immunity, so supplementation simply for these benefits is a given.
Furthermore, a wider perspective on the immune benefits of vitamin D identifies there has been persuasive research examining the effect that supplementation has on enhancing the response to vaccines for similar respiratory conditions such as influenza and that might be suggestive of a benefit to enhance the efficacy of the new Covid 19 vaccine. In the case of influenza vaccines, it appears that benefits of supplementation may be “strain” specific, with dosing prior to vaccination of certain subtype viruses delivering a higher level of immunogenic response than for others.[58] Clearly, until the Covid vaccine becomes more widely available and this effect has been evaluated, it will be impossible to predict whether this observation will be repeated in this case, and it unlikely at this early stage that vitamin D status will have been investigated as a possible “confounder” in terms of enhancing the response in current immunisation trials. Nevertheless, the ongoing use of vitamin D which helps support immunity would appear a sensible strategy. Furthermore, given that the duration or absolute level of immune protection provided by the vaccine has not been clearly defined, again maintenance of a vitamin D status that delivers a positive contribution to immunity would appear a reasonable approach.
It is also worth remembering that, harmful as it is, Covid 19 is not the only respiratory viral condition that peaks in autumn, winter and spring, and the likely relaxation of social distancing guidelines will result in more people being exposed to other infections such as influenza. Here several studies suggest that raising 25(OH)D concentrations through vitamin D supplementation in winter would reduce the risk of developing influenza as discussed in a comprehensive review of the role of vitamin D and influenza published in 2018.[59] It concluded that the evidence of vitamin D’s effects on the immune system suggest that vitamin D should reduce the risk of influenza.
Has the Covid Pandemic Simply Been a Temporary Distraction from The Real Issues Around Vitamin D Sufficiency?
The welcome likely success of the Covid Vaccine, means it is of real concern that the recent attention given to vitamin D status in UK will lose its significance and a return to the complacency relating to the subject that has so patently occurred over the past decade or more, will again become a reality. If so, this will be a significant backward step given the levels of deficiency and suboptimal vitamin D status that are currently present in UK for a number of reasons.
Firstly, this is also because there is a real need to establish the optimal level of vitamin D supplementation in specific age groups, especially the vulnerable elderly. For example, in this population one recent trial compared the effects of daily treatment with vitamin D or placebo for 1 year using blood tests of vitamin D status.[60] This was a randomized placebo-controlled trial was conducted in 305 community-dwelling people aged 65 years or older in Oxfordshire. The results demonstrated that daily 4000 IU (100mcg) vitamin D3 is required to achieve blood levels associated with lowest disease risks.
Then, consider that the UK Scientific Advisory Committee for Nutrition has set the lowest level for defining sufficiency (10 ng/ml or 25 nmol/L) of any national advisory body or scientific society and consequently recommends supplementation with 10 micrograms (400 IU) per day. Here a paper published only recently by UK researchers, highlighted that a search for published evidence to support this recommendation was completely unsuccessful.[61] They argue there is considerable evidence to support the higher level for sufficiency (20 ng/ ml or 50 nmol/L) recommended by the European Food Safety Authority and the American Institute of Medicine and hence higher dose supplementation (20 micrograms or 800 IU per day). As already highlighted given that Serum 25(OH)D concentrations in the UK typically fall by around 50% through winter, these authors believe that governments should urgently recommend supplementation with 20–25 micrograms (800–1,000 IU) per day.
The Need to Look beyond Populations and Consider Individual Needs
Whilst these higher recommendations – if adopted – should help meet the needs on a population basis, there are arguments to suggest without them – and even possibly with them – supplementation needs to be considered on a more personalized basis in order to achieve optimal status for certain individuals. Carlberg et al have identified significant inter-individual responses to supplementation, that suggest higher than currently recommended reference intakes are needed, but which can only be identified as a result of monitoring status, which many observers consider unnecessary from a cost perspective.[62] Without this, it is unlikely these individuals will benefit as they might from the correct dose of vitamin D supplementation, thereby raising the question of the cost/benefit validity of vitamin status evaluations.
Finally, there is the much-overlooked effect that medications can have on vitamin D status. Because vitamin D can be endogenously synthesised in the body and its status controlled by a number of the same cytochrome P450 enzymes (CYPs) involved in drug metabolism, this process can be affected by the use of these medications. The classes of medications that affect vitamin D status are significant and range from anticonvulsants to certain antihypertensive and diabetes drugs, as well as corticosteroids, and those used to treat gastric reflux, to name but a few.[63] Moreover, as many of these drugs are co-prescribed to treat multiple co-morbidities, especially in the elderly, their cumulative impact can further add to issues of vitamin D deficits or deficiencies. www.vitmedics.com provides a free, on-line, evidence-based tool that delivers this information in an easy to understand format.
End of Year Report-Good Progress Made in Particularly Difficult Circumstances, but 2022 Requires Even More Focus
So rather, than the Covid vaccine signalling a reduction in vitamin D research as a result of potential interest in its use in this condition waning, as demonstrated here, there is an ongoing need to understand optimal dosing not just for the wider population, but especially for specific individuals.
As Adrian Martineau (Institute of Population Health Sciences, Barts and The London, Queen Mary University of London, UK), leading the COVIDENCE UK study to investigate how diet and lifestyle factors might influence transmission of SARS-CoV-2, severity of COVID-19 symptoms, speed of recovery, and any long-term effects observes “At best vitamin D deficiency will only be one of many factors involved in determining outcome of COVID-19, but it’s a problem that could be corrected safely and cheaply; there is no downside to speak of, and good reason to think there might be a benefit”.[64]
References
- Scientific Advisory Commission on Nutrition. Rapid review: vitamin D and acute respiratory tract infections, June 2020. https://app.box.com/s/g0ldpth1upfd7fw763ew3aqa3c0pyvky .
- Covid 19 rapid evidence summary: vitamin D for covid-19 evidence summary. 29 June 2020. www.nice.org.uk/advice/es28/chapter/Key-messages .
- Royal Society. Vitamin D and covid-19. 18 June 2020. https://royalsociety.org/-/media/policy/projects/set-c/set-c-vitamin-d-and-covid-19.pdf .
- Annweiler G, Corvaisier M, Gautier J, Dubée V, Legrand E, Sacco G, Annweiler C. Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study. Nutrients. Nov;12(11):3377. 2020.
- Baktash V, Hosack T, Patel N, Shah S, Kandiah P, Van Den Abbeele K, Mandal AK, Missouris CG. Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgraduate Medical Journal. Aug 26. 2020.
- Tomasa-Irriguible TM, Bielsa-Berrocal L. Up to 40% of COVID-19 Critically Ill Patients Have Vitamin D Deficiency. Preprints. 2020.
- Dearden Jc, Rowe Ph. Correlation between vitamin D levels, individual and socio-demographic characteristics and COVID-19 infection and death rates in 20 European countries: A modelling study. The Italian Journal for Interdisciplinary Health and Social Development. Sept 30.2020.
- Pepkowitz SH, Hobel CJ, Mirocha JM, Huynh CA, Jawanda H. Vitamin D Deficiency is Associated with Increased COVID-19 Severity: Prospective Screening of At-Risk Groups is Medically Indicated. Preprint from Research Square, 29 Sep 2020.
- Beiter K, Lau FH, Danos D. Ecological association between COVID-19 deaths and vitamin D deficiency among older adults: An international country-level systematic review and analysis. PrePrints. Sept 2020.
- Karahan S, Katkat F. Impact of Serum 25 (OH) Vitamin D Level on Mortality in Patients with COVID-19 in Turkey. The journal of nutrition, health & aging. Oct 5:1-8. 2020.
- Campi I, Gennari L, Merlotti D, Mingiano C, Frosali A, Giovanelli L, Torlasco C, Pengo MF, Heilbron F, Soranna D, Zambon A. Vitamin D and COVID-19 Severity and Related Mortality: A Prospective Study in Italy. Preprints Sept 2020.
- Abrishami A, Dalili N, Torbati PM, Asgari R, Arab-Ahmadi M, Behnam B, Sanei-Taheri M. Possible association of vitamin D status with lung involvement and outcome in patients with COVID-19: a retrospective study. European Journal of Nutrition. Oct 30:1-9. 2020.
- Hamza A, Ahmed M, Ahmed K. Role of Vitamin D in Pathogenesis and Severity of Coronavirus Disease 2019 (COVID-19) Infection. J.M.H.S Vol14. Apr-Jun 2020.
- Annweiler C, Hanotte B, de l’Eprevier CG, Sabatier JM, Lafaie L, Célarier T. Vitamin D and survival in COVID-19 patients: A quasi-experimental study. The Journal of Steroid Biochemistry and Molecular Biology. Oct 13:105771.2020.
- Ling SF, Broad E, Murphy R, Pappachan JM, Pardesi-Newton S, Kong MF, Jude EB. Vitamin D Treatment Is Associated with Reduced Risk of Mortality in Patients with COVID-19: A Cross-Sectional Multi-Centre Observational Study. Available at SSRN 3690902.
- Radujkovic A, Hippchen T, Tiwari-Heckler S, Dreher S, Boxberger M, Merle U. Vitamin D deficiency and outcome of COVID-19 patients. Nutrients. Sep;12(9):2757. 2020.
- Pizzini A, Aichner M, Sahanic S, Böhm A, Egger A, Hoermann G, Kurz K, Widmann G, Bellmann-Weiler R, Weiss G, Tancevski I. Impact of vitamin D deficiency on COVID-19—A prospective analysis from the covild registry. Nutrients. Sep;12(9):2775. 2020.
- Macaya F, Paeres CE, Carbó AV, Fernández-Ortiz A, Del Castillo JG, Sánchez FJ, de la Vega IR, Herrera MA. Interaction between age and vitamin D deficiency in severe COVID-19 infectio Nutrición hospitalaria: Organo oficial de la Sociedad española de nutrición parenteral y enteral. (5):1039-42. 2020.
- Kaufman HW, Niles JK, Kroll MH, Bi C, Holick MF. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PloS one. Sep 17;15(9):e0239252. 2020.
- Maghbooli Z, Sahraian MA, Ebrahimi M, Pazoki M, Kafan S, Tabriz HM, Hadadi A, Montazeri M, Nasiri M, Shirvani A, Holick MF. Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PloS one. Sep 25;15(9):e0239799. 2020.
- Castillo ME, Costa LM, Barrios JM, Díaz JF, Miranda JL, Bouillon R, Gomez JM. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. The Journal of steroid biochemistry and molecular biology. 2020 Oct 1;203:105751.
- Laird E, Rhodes J, Kenny RA. Vitamin D and inflammation: potential implications for severity of COVID-19. Ir Med J. 7;113(5):81. 2020.
- D’Avolio A, Avataneo V, Manca A, Cusato J, De Nicolò A, Lucchini R, Keller F, Cantù M. 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2. Nutrients. May;12(5):1359.2020.
- Pereira M, Dantas Damascena A, Galvão Azevedo LM, de Almeida Oliveira T, da Mota Santana J. Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis. Critical Reviews in Food Science and Nutrition. Nov 3:1-9. 2020.
- Ferrari D, Locatelli M. No significant association between vitamin D and COVID-19. A retrospective study from a northern Italian hospital. PrePrints. Sept 2020.
- Ghasemian R et al, The Role of Vitamin D in The Age of COVID-19: A Systematic Review and Meta-Analysis Along with an Ecological Approach doi: https://doi.org/10.1101/2020.06.05.20123554 medRxiv preprint
- Davies G et al. Evidence Supports a Causal Role for Vitamin D Status in Global COVID-19 Outcomes. medRxiv preprint doi: https://doi.org/10.1101/2020.05.01.20087965
- Daneshkhah A et al. The Role of Vitamin D in Suppressing Cytokine Storm in COVID-19 Patients and Associated Mortality medRxiv preprint doi: https://doi.org/10.1101/2020.04.08.20058578
- Kara M, Ekiz T, Ricci V, Kara Ö, Chang KV, Özçakar L. ‘Scientific Strabismus’ or Two Related Pandemics: COVID-19 & Vitamin D Deficiency. British Journal of Nutrition. Jan 1:1-20. 2020.
- Rhodes JM et al. low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity. Alimentary pharmacology & therapeutics. Jun;51(12):1434-7. 2020.
- Ferrari D, Locatelli M, Briguglio M, Lombardi G. Is there a link between vitamin D status, SARS‐CoV‐2 infection risk and COVID‐19 severity?. Cell Biochemistry and Function. Nov 2. 2020.
- Grant WB et al. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths Nutrients 12, 988. 2020.
- Singh S, Kaur R, Singh RK. Revisiting the role of vitamin D levels in the prevention of COVID-19 infection and mortality in European countries post infections peak. Preprints Sept 2020.
- Cuñat T et al. Vitamin D deficiency in critically ill patients diagnosed with COVID -19. Are we doing enough? A retrospective analysis of 226 patients., https://doi.org/10.21203/rs.3.rs-30390/v1+
- De Smet et al. Vitamin D deficiency as risk factor for severe 1 COVID-19: a convergence of two pandemics. medRxiv preprint doi: https://doi.org/10.1101/2020.05.01.20079376
- Cristian P et al. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clinical and Experimental Research https://doi.org/10.1007/s40520-020-01570-8
- Lau F et al. Vitamin D insufficiency is prevalent in severe COVID-19 medRxiv preprint doi: https://doi.org/10.1101/2020.04.24.20075838
- Meltzer D et al. Association of Vitamin D Deficiency and Treatment with COVID-19 Incidence doi: https://doi.org/10.1101/2020.05.08.20095893 medRxiv preprint
- Skutsch, M. et al. The association of UV with rates of COVID‐19 transmission and deaths in Mexico: the possible mediating role of vitamin D. medRxiv preprint doi: https://doi.org/10.1101/2020.05.25.20112805
- Pinzon R et al. Vitamin D Deficiency Among Patients with COVID-19;Case Series and Recent Literature Review, 21 May 2020, PREPRINT (Version 1).
- Raharusun P. Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study. Available at SSRN 3585561. Apr 26. 2020.
- Alipio M et al. Vitamin D supplementation could possibly improve clinical outcomes of patients infected with Coronavirus-2019 (COVID-2019) Preprints April 9, 2020.
- Darling A et al. Vitamin D status, body mass index, ethnicity and COVID-19: Initial analysis of the first-reported UK Biobank COVID-19 positive cases (n 580) compared with negative controls (n 723) doi: https://doi.org/10.1101/2020.04.29.20084277 medRxiv preprint
- Hastie CE et al. Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 14. 561e565.2020.
- Ebadi M et al. Nutrition in acute and chronic diseases Perspective: improving vitamin D status in the management of COVID-19. European Journal of Clinical Nutrition 74:856–859. 2020.
- Isaia G, Medico E. [Possible prevention and therapeutic role of vitamin D in the management of the COVID-19 2020 pandemics]. Torino (ITA): University of Turin; 2020.
- Weir EK et al.Does vitamin D deficiency increase the severity of COVID-19? Clinical Medicine 2020 Vol 20, No 4 July 2020.
- Chakhtoura Commentary: Myths and facts on vitamin D amidst the COVID- 19 pandemic. Metabolism Clinical and Experimental 109. 154276. 2020.
- Carter S et al. Considerations for Obesity, Vitamin D, and Physical Activity Amid the COVID-19 Pandemic.The Obesity Society. doi:10.1002/oby.22838.
- Meltzer DO, Best TJ, Zhang H, Vokes T, Arora V, Solway J. Association of vitamin D status and other clinical characteristics with COVID-19 test results. JAMA network open. Sep 1;3(9):e2019722. 2020.
- Alipio M. Vitamin D Supplementation Could Possibly Improve Clinical Outcomes of Patients Infected with Coronavirus-2019 (COVID-19). Available at SSRN 3571484. 2020 Apr 9.
- Merzon E, Tworowski D, Gorohovski A, Vinker S, Golan Cohen A, Green I, Frenkel‐Morgenstern M. Low plasma 25 (OH) vitamin D level is associated with increased risk of COVID‐19 infection: an Israeli population‐based study. The FEBS journal. Sep;287(17):3693-702. 2020.
- El James Glicio MD, Neelam S, Rashi R, Ramya D. Vitamin D Level of Mild and Severe Elderly Cases of COVID-19: A Preliminary Report. review and meta-analysis. Apr;10(4):409. 2020.
- Roberts C, Steer T, Maplethorpe N et al. National Diet and Nutrition Survey Results from Years 7 and 8 (combined) of the Rolling Programme (2014/2015 to 2015/2016). PHE publications. Available at: https://www.gov.uk/government/statistics/ndnsresults - from-years-7-and-8-combined
- PHE (Public Health England) (2016) Press release: PHE publishes new advice on vitamin D. Available at: https://www.gov.uk/government/news/phe-publishes-new-advice-on-vitamin-d
- SACN (Scientific Advisory Committee on Nutrition) (2016) Vitamin D and health. Available at: https://www.gov.uk/government/publications/sacn-vitamin-d-and-health-report .
- O’Connor C, Glatt D, White L, Revuelta Iniesta R. Knowledge, attitudes and perceptions towards vitamin D in a UK adult population: a cross-sectional study. International journal of environmental research and public health. Nov;15(11):2387. 2018.
- Lee MD, Lin CH, Lei WT, Chang HY, Lee HC, Yeung CY, Chiu NC, Chi H, Liu JM, Hsu RJ, Cheng YJ. Does vitamin D deficiency affect the immunogenic responses to influenza vaccination? A systematic review and meta-analysis. Nutrients. Apr;10(4):409. 2018.
- Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, Bhattoa HP. 32252338 Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and Covid-19 Infections and Deaths Nutrients Apr. 2 12 (4).988.2020.
- Hin H, Tomson J, Newman C, Kurien R, Lay M, Cox J, Sayer J, Hill M, Emberson J, Armitage J, Clarke R. Optimum dose of vitamin D for disease prevention in older people: BEST-D trial of vitamin D in primary care. Osteoporosis International. Mar 1;28(3):841-51. 2017.
- Griffin G, Hewison M, Hopkin J, Kenny RA, Quinton R, Rhodes J, Thickett D. Preventing vitamin D deficiency during the COVID-19 pandemic: UK definitions of vitamin D sufficiency and recommended supplement dose are set too low. Clinical Medicine. Nov 6. 2020.
- Carlberg C, Haq A. The concept of the personal vitamin D response index. The Journal of steroid biochemistry and molecular biology. Jan 1;175:12-7. 2018.
- van Orten-Luiten AC, Janse A, Donukshe-Rutten RA, Witkamp RF. The associations between drug use, indicators of nutritional status and vitamin d levels, a cross-sectional analysis of a polypharmaceutical geriatric outpatient population. European Geriatric Medicine. (4):S134. 2013.
- Mitchel F, Vitamin-D and COVID-19: do deficient risk a poorer outcome? thelancet.com/diabetes-endocrinology Vol 8 July 2020
Comments:
-
Tom said..
As of now, there are 3-4 "vaccines" which are not traditional vaccines at all with dozens more on the way in the US and EU. These potions are gene editing/replacement therapies or made from adenovirus (common cold) derivatives. For the most part, your immune system is being told to manufacture specific spike proteins that may or may not be able to fight SARS CoV-2. Since there was so little testing and the trials were so flimsy, there is no way of knowing much of anything about these concoctions.
Avoid the injections and pay more attention to vitamin and mineral intake and eating a healthier diet. I would never trust pharma's new experimental potions to be even close to anything my own immune system can create to fight infections or viruses. And the real sticking point has to be the question of having billions of new proteins foreign your body and what they will do in the long run. That will not be known for at least 5-10 years.