Positive Health Online
Your Country

Dental Posture Interactions for Optimal Health
by Malcolm Levinkind(more info)
listed in dentistry, originally published in issue 88 - May 2003
Introduction
The concept that good health is related in some way to posture is not new to Eastern or Western health philosophies. It has been established that dental health can have an impact on general health.[1],[2] However, for many people, the possibility that their dental bite can influence posture and therefore their health is a thought-provoking idea.
The aims of this article are to present some of the key evidence that dental occlusion (bite) can influence an individual's posture and put forward the case for making an objective postural assessment which includes evaluation of occlusion as an essential part of the clinical management of postural problems.
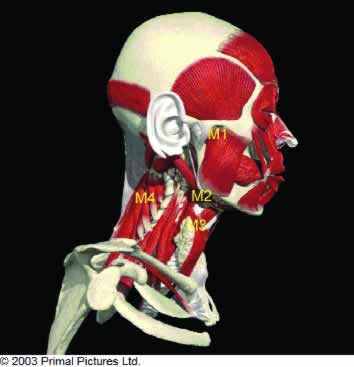
Figure 1. Image showing head and neck with groups of muscles.
M1 closing mouth. M2 Supra hyoid muscles opening mouth and head posture forwards.
M3 Infa hyoid muscles, opening mouth and head posture forwards.
M4 Neck muscles, head posture backwards.
Some General Thoughts About Posture
Good posture in humans is seen when the head is supported by the vertebral column which in turn is supported by the pelvis, legs and feet. The arms are suspended from the individual's shoulders, which are level with respect to the pelvis and feet. The individual's centre of gravity is situated within the body such that their weight is distributed evenly through all the vertebrae and the person is comfortable. The feet are at the centre of the physical forces acting upon the body whilst standing. Maintenance of an erect head posture depends upon the interaction between gravity and the muscles, bones and joints, all of which are coordinated by the individual's nervous system.
In cases of poor posture, one of the patterns seen commonly involves the centre of gravity being projected forward, usually due to the head being held forward, anterior to the vertebral column. This places a strain on the muscles of the neck, shoulders and lower back and if symptoms occur they will be noted to involve the vertebrae of the neck and lower back. Whether symptoms occur, and their exact site, is dependant upon several factors that include the duration of the compensated posture and the individual's ability to tolerate the adaptation.
What Drives Posture?
If one considers the human body as a closed mechanical system, the genetic make-up of an individual will dictate their body shape and musculo-skeletal composition. As a baby, posture is controlled by reflex coordination of the neuromotor system.[3] These reflexes, which are developed in utero, are pre-programmed responses to stimuli and are designed to aid survival. As growth, development and maturation proceed there are underlying reflexes that provide support for body functions, and as they mature they provide the foundations for voluntary and coordinated movements to take place. If there are any imbalances, for example, if there is a problem with one of the joints, there will be some sort of compensation in order to maintain the overall stability of the system. So, any observed postural changes will result from the interaction between the genetic and environmental factors.
If an adjustment takes place in one part, for example as a result of a stone in your shoe, compensations will take place as you walk in order to maintain stability of your posture. If the stone is left in your shoe, the position of the stone in your shoe will determine the actual compensation that will result. This change in posture, which if maintained over any length of time, may cause symptoms distant to the foot under which the stone was placed. In addition, there may be a specific local effect, in this particular case, formation of a blister. This hypothetical situation can be considered as an ascending effect caused by an environmental factor. The possibility of descending effects, specifically the interaction between cranial factors including bite and changes in posture, must also be considered. The simplest explanation for a descending factor altering body posture is that it is caused by changes in head posture, as the head has to be balanced on the neck and supported by the pelvis, legs and feet.
An Overview of the Relevant Anatomy of the Head and Neck
Figure 1 shows a stylized view of the bones of the head and neck with the various groups of muscles involved in maintaining its posture and function. There are antagonistic groups of muscles that are responsible for the opening and closing movements of the mouth that facilitate breathing, chewing, swallowing and speech. The muscles responsible for closing the mouth are attached above the mandible, via tendons, to the skull. Those muscles below the mandible are anatomically described as being above or below the hyoid bone and together with gravity, are responsible for opening the mouth. The tongue is suspended from the inside of the mandible above the hyoid bone and has muscles with a range of different orientations. These facilitate changes in its shape and together with the surrounding muscles control its position.
The atlanto-occipital (A-O) joints are a pair of synovial joints contributed to by the occipital bone, which forms part of the base of the human skull and the first neck or cervical vertebra called the 'Atlas'. This arrangement is unique in the neck as there are only two articular facets, whereas all the other cervical vertebrae have three articular facets. Both sliding movements[4] and rotations[5] take place at this joint.
The lower jaw or mandible articulates with the skull via the pair of tempempero-mandibular joints (TMJs) with the temporal bones, within which the sensory centres for hearing and balance (auditory and vestibular apparatus) are housed. The TMJs have a piece of cartilage interposed between the articular head of the mandible, the condyle and the base of the skull. The movement of the mandible involves not only hinge-type rotation but, also a sliding motion at the TMJs.
There is a considerable amount of standard anatomical literature that describes the 22 bones of the skull and the shapes of the joints (sutures) and the 106 different articulations. Kragt et al[6] showed that movement was possible at the sutures in macerated human skulls and Retzlaff at al[7] documented that the cranial sutures do not fuse with age. Prichard et al[8] concluded that "it may be deduced from their mode of development and their histological organisation, that sutures form a strong bond of union between the adjacent bones, while permitting slight movement." The possible association between motion of the cranial bones and restorative dentistry was reviewed by Libin,[9] who concluded that the cranial mechanism offers dentists an added dimension for solving and avoiding clinical problems.
Tooth position is determined by the position of the supporting bone and pressure from the surrounding soft tissues. They occupy a 'neutral' zone determined by forces from the tongue inside the mouth and the cheeks and lips outside the mouth. Local factors such as sucking habits, for example a thumb or pencil, or wearing an orthodontic appliance will alter tooth position and can change soft tissue shape and function as well.
Linking Head Posture and Bite
Head posture and bite are intimately related. It has been shown that head posture can influence initial tooth contacts[10] You can do an experiment by bending your head forwards, biting together and notice how your bite feels. Stop biting your teeth together, now tilt your head back fully and bite again. Notice the difference in how your bite feels. Maintenance of head posture depends upon the interaction between the effects of gravity and the balance between the muscles that stabilize the head. If we consider that the teeth provide the balancing contact for stability of head posture, it is possible that changes in our bite will have an effect as well. A non-ideal arrangement of the teeth is called a malocclusion. A normal bite of occlusion is called a Class I. When the upper jaw is more in advance than the lower jaw than average, this is termed a Class II, and if the lower jaw is positioned in advance of the upper jaw this is termed a Class III.
Using a balance platform it has been shown that subjects with Class II malocclusion exhibit an anteriorly displaced posture, whereas subjects with a Class III malocclusion exhibited a posteriorly displaced posture.[11] When investigating the posture adopted by the cervical vertebrae, it was reported that nearly half the patients with a Class I or Class II had a marked cervical lordosis (arching forward) whereas Class III had abnormal kyphosis (arching backwards). The Class I and Class II patients benefitted from treatment but Class III did not.[12]
When comparing Class I and with Class III malocclusions, the position and inclination of the hyoid bone was found to be more anterior and it had a reversed inclination. The implications of this research were that malocclusion can influence supra- and infra-hyoid muscle function and affect the direction of mandibular growth.[13]
Patients with severe malocclusions have most commonly been found to have a head and neck forwards posture. This forward head and neck posture has been significantly correlated with the Class II skeletal pattern.[14]
A review of the dental literature carried out by Woda et al reported that mandibular position is constantly variable, and that mandibular posture greatly depends upon head posture.[15]
Compensations in Head and Neck Posture That Can Cause Pathological Changes
Given that it is possible for movement to occur at the AO joints, temperomandibular joints, sutures of the skull and hyoid bone, it is not so surprising to find that compensations may occur which can lead to symptoms. Although teeth make micro-movements in their sockets, and the amount of movement at the cranial sutures is limited, most of the compensations that can take place tend to occur at the AO joints, in the TMJs, the hyoid bone, vertebrae or the surrounding soft tissues. Faulty position of the cartilage between the head of the condyles and the base of the temporal bones can lead to clicking or popping noises from the jaw joints when patients experience symptoms from their TMJs.
Altered head and neck posture is often the cause of TMJ problems.[16] Patients with a malocclusion compensate by altering the normal masticatory muscle function, perhaps facilitating cervical spine disorders. Some of the other symptoms such as tinnitus and vertigo may be due to the fact that the vestibular (balance) and auditory (hearing) centres are located in the temporal bones. Other symptoms distant from the head and neck may be linked to descending problems but may not be apparent unless assessed specifically.
How to Assess Posture
To establish the correct diagnosis may involve a combination of conventional and complementary techniques. If the therapist or clinician assesses posture visually and makes a written record, this is a subjective assessment and, although it may not be fully detailed, can provide a reasonable assessment. It has been shown that photographs provide a reliable way to evaluate posture and this is an objective, repeatable method.[17] With the introduction of affordable digital cameras this is likely to become the method of choice in the future. The general body postural assessment system that is used in my clinic involves two mirrors, one above and one at the side of the person being assessed. Both these mirrors are angled so that the digital camera, which is a fixed distance from the subject, can see the vertex and side view at the same time as a back or front view, and only two images are needed to evaluate the gross static posture (Figures 2 and 3). To carry out a cranial assessment, the patient's head is placed in a cephalostat. This device uses short conical plastic tubes, which are inserted into the ears to produce a 'relative' horizontal plane, in turn making the ears parallel to the floor (Figure 4). All other facial planes are then measured relative to the ear plane. Once the postural images have been assessed it is then possible to decide if any other tests such as x-ray pictures may be appropriate to aid the diagnosis and help plan treatment.
Case Report: 1
An example of an ascending problem that was 'locked in' by the bite is shown in Figures 2, 3 and 4. This patient was referred by his osteopath, who reported that she could not correct this young man's pelvis any further and wondered if his bite was contributing to his symptoms. The initial clinical assessment showed that the patient had major postural compensations. He had a deep bite and there was a pattern suggesting that his temperomandibular joints were involved. The effects of his dental splint therapy are shown following treatment for one month (Figure 5) and after three months (Figure 6). The dental treatment allowed spontaneous correction of the patient's pelvis as there was no osteopathic input during the three months of dental splint therapy.
Management of Bite and Postural Problems
There is a growing awareness amongst healthcare workers that patients often require multi-disciplinary input to help them attain optimal health. The key issues are to ensure that the correct diagnosis is made and to integrate not only the provision of appropriate therapies but also to coordinate the way that the treatment is administered.
Although conventionally and complementarily trained clinicians and therapists are well qualified and may have many years of experience, they often concentrate on just their area of expertise. If a truly holistic approach were to be taken in relation to managing postural problems, regardless of the therapist's speciality, ideally posture should be quantified before, during and after treatment. When evaluated before treatment this can help determine whether there is a postural component contributing to an individual's symptoms, and which aspect of the posture is the key component. During treatment, a postural evaluation will ensure that the postural problems are being managed appropriately. Finally as maintenance of health is a very important aspect of optimal health, postural evaluation can provide motivation and feedback which will allow an individual to 'help themselves' and not rely entirely on further therapeutic input from others.
Correct treatment of any clinical problem must be based on making the correct diagnosis, the confirmation of which is then aided by the use of special tests such as radiographs and blood tests. The management of postural problems is no different. Often patients will be having their symptoms treated and this will provide some relief, but not actually solve their problems. Assessment of bite in relation to postural problems, prior to treatment, will ensure that the correct treatment is carried out.
For example, it has been reported that postural and muscle function abnormalities appeared to be more common in patients with temperomandibular disorders, and if they do not respond to dental splint therapy, the interaction between their posture and muscular function should be investigated.[18]
Case Report: 2
An example of a descending dental cause of postural changes is shown in Figure 7, in which the patient's head is tilted to her left. This 7-yearold girl presented with an abscess associated with her upper right first baby molar (Figure 8). Her postural pattern is what would be expected if she had altered her bite as a result of pain from the abscessed tooth. Her abscess had been present for several weeks and management had been based on the use of antibiotics alone. This had not completely resolved her symptoms, which included inability to chew on her right side. After resolving her abscess by removing the tooth and balancing the extraction by also removing the contra-lateral baby molar (Figure 9), the photograph taken at her follow up visit, four days later showed that her head tilt was resolved (Figure 10) and she was no longer experiencing discomfort from her mouth.
References
1. Mattila KJ et al. Association between dental health and acute myocardial infarction. Br Med J. 298: 779-782. 1989.
2. Österberg T, Mellström D and Sundh V. Dental health and functional ageing. A study of 70-year-old people. Community Dent & Oral Epidemiol. 18: 313-318. 1990.
3. Paine R. The evolution of infantile postural reflexes in the presence of chronic syndromes. Dev Med Child Neurol. 6: 345. 1964.
4. Makofsky HW. The effect of head posture on muscle contact position: the sliding cranium theory. J Craniomandibular Practice. 7: 268-292. 1989.
5. Punjabi M et al. Three dimensional movements of the upper cervical spine. 13: 726-730. 1988.
6. Kragt G, Bosch JJ and Borsboom PCF. Measurement of bone displacement in a macerated human skull induced by orthodontic forces; a holographic study. J Biomechanics. 12: 905-910. 1979.
7. Retzlaff EW et al. Age related changes in human cranial sutures. Anatomic Records. 663. 1979.
8. Prichard JJ. Structure and development of cranial and facial sutures. J Anat. 90: 73-86. 1956.
9. Libin BM. The cranial mechanism: its relationship to cranial-mandibular function. J Prosthetic Dentistry. 58(5): 632-638. 1987.
10. Chapman RJ et al. Occlusal contact variation with changes in head position. Int J Prosthodont. 4: 377-381 1991.
11. Nobili A and Adversi R. Relationship between Posture and Occlusion: A clinical and experimental investigation. J Craniomandibular Practice. 14: 274-285. 1996.
12. Martensmeir I and Dietrich P. Which correlations between cervical posture and malocclusions. Fortschr Kieferothop. 52: 26-32. 1992.
13. Adamidis IP and Spyropoulos M. Hyoid bone position and orientation in Class I and Class III malocclusions. Am J Orthod Dentofac Orthop. 101: 308-312. 1992.
14. Capurso U et al. Parametri posturali cefalometrci e malocclusioni dentari. Mondo Ortod. 14: 345-349. 1989.
15. Wooda A et al. Critical reviews in Oral Biology & Medicine. 12: 166-178. 2001.
16. Tallgren A et al. Changes in jaw relation, hyoid position, and head posture in complete denture wearers. J Prosthet Dent. 50: 148-156. 1983.
17. Zonnenberg AJJ et al. Body postural photographs as a diagnostic aid for musculoskeletal disorders related to temperomandibular disorders. J Craniomandibular Practice. 14(3): 225-232. 1996.
18. Wright E et al. Usefulness of postural training for patients with temperopmandibular disorders. J Am Dent Assoc. 131: 202-210. 2000.
The author thanks Primal Pictures Ltd (www.primalpictures.com) for their permission to use and modify their artwork in Figure 1.
Comments:
-
No Article Comments available