Positive Health Online
Your Country

How Rothbarts Foot Leads to Poor Posture and Chronic Pain
by Brian A Rothbart PhD(more info)
listed in bodywork, originally published in issue 211 - January 2014
Abstract
The talar bone (seated on top of the foot’s heel bone), goes through a series of growth changes that reshapes the contour of the forefoot. At approximately week five post ovulation, the talar head is untwisting around its longitudinal axis.[10-12] If this ‘torsional growth’ in the talar head ends prematurely, the 1st metatarsal, proximal phalanx and hallux (e.g.1st ray) remain in supinatus (structurally elevated and inverted).
Postnatally, when standing; gravity pulls the elevated 1st ray downward to the ground. As the 1st ray collapses to the ground, the body shifts into a kyphotic posture. As a result, weight bearing joints become mal-aligned and postural muscles compensate by tightening. In time, these joint and muscle changes lead the patient into chronic, debilitating musculoskeletal pain, foot to jaw.
1. Introduction
Postural distortions (poor posture) have been linked to chronic muscle and joint pain by many authors. However, the cause of the postural distortions is still highly debated with multifaceted aetiologies being suggested.[1-8]
Rothbart[9] described a previously unrecognized foot structure in which the 1st ray (first metatarsal, proximal phalanx and hallux) are structurally elevated and inverted. Rothbart terms this foot structure Primus Metatarsus Supinatus (PMS), now commonly called Rothbarts Foot, which he links to the development of a kyphotic posture.
This paper discusses the embryogenesis of PMS, the series of postural shifts resulting from PMS, and the link between these postural shifts and chronic musculoskeletal pain.

Figure 1 – Angular variances in the torsion of the talar head (red and blue arrows) and
inward twist of the 1st metatarsal and big toe (proximal phalanx and hallux)
2. Talar Torsion Linked to Primus Metatarsus Supinatus
Sewell[13] was the first to publish on the substantial variances in the torsion of the talar head. Straus[14] reported similar angular variances in this torsion, ranging from 26 to 43 degrees, McPoil et al[15] from 24 to 51 degrees, and Sarrafian[16] from 30 to 65 degrees (see Figure 1). Tax [17] and Hlavac [18] proposed that talar torsion may determine the structural position of the forefoot. Daniel [19], in an in vitro cadaver study, demonstrated that angular changes in the structure of the talar bone visibly changed the shape of the forefoot.
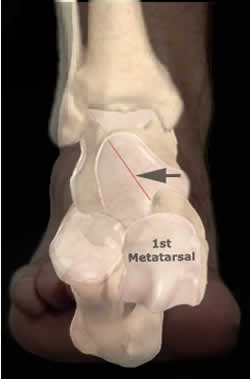
Figure 2 – Complete unwinding of the talar head (black arrow) results in a plantargrade foot
(no structural elevation or twist in the 1st metatarsal and big toe
Rothbart suggests that if talar torsion is GREATER than 35 degrees this results in a planter grade foot. That is when the subtalar joint is placed in its anatomical neutral position, the entire forefoot rests on the ground. (See Figure 2)

Figure 3 – Retention of talar supinatus (black arrow) results in the structural elevation
Rothbart also suggests that if the talar torsion is LESS than 35 degrees, when the subtalar joint is in its anatomical neutral position, the 1st metatarsal and hallux do not rest on the ground. Instead, they are twisted inward and upward relative to the 2nd metatarsal. Rothbart terms this foot structure as Primus Metatarsus Supinatus PMS (Rothbarts) Foot. (See Figure 3)
PMS typically has a flexible inner longitudinal arch (higher when sitting, lower when standing). Gait analysis reveals a strong ‘supinatory’ strike at heel contact (accounting for the lateral heel wear patterns) and abnormal pronatory rotation (inward and downward) at mid-stance. This unlocks the forefoot and allows the elevated 1st metatarsal and hallux (driven by gravity) to fall to the ground. Thus the elevated 1st metatarsal and hallux are not manifested when standing or walking.

Figure 4 – Rothbarts Foot can be quantified using BioVectors underneath the foot. Triangular
wedges are placed underneath the first metatarsal and hallux. The degree of supinatus (elevation of the
first metatarsal and hallux) can be read directly off the BioVector
This structural alteration becomes apparent when the foot is placed in its anatomical neutral position (See Figure 4) and can be quantified using biovectors (calibrated wedges) underneath the feet. Biovectors are used to quantify, in millimetres, the distance between the ground and the elevated 1st metatarsal head . This distance is referred to as the Primus Metatarsus Supinatus value (PMSv). This measuring technique was found to have a high inter and intra rater reliability in a double blind study conducted at Georgia University.[20]
Ascertaining the PMSv in infants under four years of age is difficult and prone to error due to the budding longitudinal fat pad and the late ossification of the navicular bone (typically around the age of four). However, as the longitudinal fat pad attenuates and the navicular bone ossifies, PMSv becomes as easy to accurately ascertain as taking a radial pulse. PMSv between 11mm and 24mm are pathognomonic of PMS and are frequently used in the differential diagnosis.
3. PMS and the Development of the Kyphotic Posture
PMS is a common precursor to the development of the kyphotic posture. Two distinct models have been suggested that explain this link.
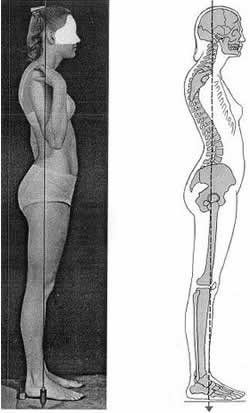
Figure 5 – Kyphotic Posture. The most common postural distortional pattern linked to Rothbarts Foot
The BioMechanical Model
In a strong gravitational field (i.e., Mother Earth), PMS forces the weight-bearing foot to roll inward, forward and downward (pronate) until the 1st metatarsal rests on the ground. It is theorized that this pattern of foot pronation shifts the body’s centre of gravity forward and downward, which in turn, pulls the innominates forward and downward. This can unlevel the pelvis and result in a functional leg length discrepancy.[21] As these displacements cascade up the axial framework, scoliotic and kyphotic curves increase and may become unstable. The thoracic cage twists and the shoulders protract.[22] Typically, the head is thrust forward, the maxilla moves anteriorly (relative to the mandible) resulting in a Class II malocclusion.[23] This gravity-induced skeletal ‘collapse’ was originally termed BioImplosion,[23] but now is more correctly referred to as a kyphotic posture (See Figure 5).
The BioMechanical Model was first introduced by Root in the mid 1950s to explain lower body mechanics and then later expanded by Rothbart to include upper body mechanics.[32] The BioMechanical Model provides a very logical and intuitive explanation on how PMS leads to a kyphotic posture.
The Neurophysiological Model
An introduction to the Neurophysiological Model can be shown by the following exercise, which visually depicts the interconnection between the extremities and the brain. That is, changing motion or position in one part of the body (such as the feet), changes motion or position in other parts of the body, all this being coordinated through the central nervous system (brain).
- Sitting at your desk, lift your right foot off the floor and draw clockwise circles with the foot;
- While maintaining this foot motion; in a counter clockwise direction, draw the number ‘6’ in the air with your right hand;
- The foot will automatically change directions (clockwise to counter-clockwise).
The Foot to Brain Connection[26-29]
The Neurophysiological Model that Rothbart suggests is a foot to brain connection that dramatically affects the posture:
The plantar surfaces of the feet are embedded with millions of fast acting touch receptors (Meissner’s corpuscles). In a closed kinetic chain, at any given moment, certain areas of the foot are touching the ground. At each point of contact, the Meissner corpuscles are being stimulated. When a group of Meissner corpuscles are simultaneously stimulated, it is referred to as a pattern of stimulation.
Rothbart has found that in PMS (a twisting or excessively pronating foot), the patterns of stimulation are distorted compared to the patterns of stimulation in a non-twisting foot. That is:
- In a non-twisting foot, the Meissner’s corpuscles are stimulated evenly across the heel and ball of the foot (e.g., a non-distorted pattern of stimulation);
- In PMS, the Meissner’s corpuscles are stimulated along the outside of the heel and inside of the ball of the foot (e.g., a distorted pattern of stimulation).
Patterns of stimulation which are formed in the feet send signals to the cerebellum. These signals provide the cerebellum with a picture of where the body is in space (e.g., the body’s posture). Based on these signals, the cerebellum is constantly readjusting the body’s position in order to maintain an upright and stable posture.
- Patterns of stimulation formed by a non-twisting foot send non-distorted signals to the cerebellum. From these non-distorted signals, the cerebellum automatically maintains a non-distorted posture;
- Patterns of stimulation formed by a PMS send distorted signals to the cerebellum. From these faulty signals, the cerebellum automatically maintains a kyphotic posture.
Rothbart (2009) suggests that the higher the big toe is elevated off the ground (e.g., as the severity of PMS increases), the greater the foot twists. The greater the foot twist, the greater the distortion in the patterns of stimulation and resulting signals to the cerebellum. The more distorted the signals, the worse the kyphotic posture.
The neurophysiological model was introduced by Rothbart in 2002. He developed this new paradigm because the biomechanical model did not explain what he was seeing clinically through his use of proprioceptive insoles. That is, by applying proprioceptive (non-supporting) stimulation under the feet, dramatic postural changes were achieved.
The Neurophysiological Model explains how non-supportive type insoles can dramatically change posture and suggests that the only way to effectively eliminate chronic muscle and joint pain is to change the distorted patterns of stimulation to a non-distorted pattern. The cerebellum automatically responds by reversing the kyphotic posture towards a non-distorted posture.
 Figure 6 – 17 year old Downs female – note the shoulder protraction and dramatic forward position of the head |
 Figure 7 – Note the dramatic improvement in posture which occurs almost instan- taneously when the patient stands on the proprioceptive insoles (retraction of shoulders, reversal of forward head position) |
The biomechanical model implies that rigid or semi-rigid orthotics must be used to support the feet if one wishes to reverse the kyphotic postures resulting from PMS. But, this implication belies the effectiveness of the newer generation of proprioceptive insoles[25] which do not support the feet, but which do reverse the kyphotic postures resulting from PMS (See Figures 6 and 7).
4. Resulting Muscle and Joint Pain
A non-distorted posture maintains correct alignment and healthy cartilage within the weight-bearing joints, so they remain healthy, mobile and pain free. The muscles function optimally and do not become overly tight or stretched.

Figure 8 – Osteodegenerative Arthritis of the knee. The medial joint space (white arrow) is
narrowed due to compression of the cartilage. This is thought to result from a postural distortion that
shifts the body’s weight through the inside of the knee
Conversely, the kyphotic posture, resulting from PMS, has been linked to joint inflammation and muscle hypertonicity: When the weight bearing joints are out of alignment (e.g., kyphotic posture), the body’s weight is distributed unevenly across these joints (ankles, knees, hips, back, neck and jaw). This uneven weight distribution results in uneven wear patterns within the cartilaginous caps (See Figure 8). The joints become arthritic (osteodegenerative arthritis) and eventually painful.
The kyphotic posture resulting from PMS has also been linked to increased muscle tightness (hypertonicity). That is, the body overuses muscles across positionally unstable joints to maintain an upright posture. This constant reliance on muscles to stabilize the joints is very fatiguing on the body and may be an important factor in the development of Fibromyalgia and Chronic Fatigue Syndrome.
Visceral components have also been noted in some patients with kyphotic posture.[31] In theory, because the internal organs ‘hang’ on the skeletal framework, torsion of the skeleton can produce compression and/or torsion on the viscera. To use another example from engineering, if a building ‘severely settles’, the doors and windows may jam, plumbing problems may arise and the roof may leak. Similarly, it is not surprising for patients with an anterior rotation of the pelvis to have a ‘tipped’ uterus and/or suffer from gastrointestinal or urogenital problems. And it is not surprising for patients with a severe forward head position to have sinus and occlusal problems.
5. Summary
PMS is a very common embryological foot structure which functionally excessively pronates (twists). This excessive foot pronation results in a kyphotic posture.
One explanation on how this occurs is offered by the BioMechanical Model. Gravity distorts the body’s posture similar to the way it disrupts the stability of a building with an unstable foundation.
Another explanation is offered by the Neurophysiological Model: Distorted patterns of stimulation are generated by a twisting foot. These distorted patterns result in distorted signals to the cerebellum. Acting on these distorted signals, the cerebellum automatically maintains a kyphotic posture.
Both models result in the same clinical picture: the weight bearing joints become mal-aligned. The postural muscles compensate for this joint mal-alignment by tightening up across these joints. This combination of joint mal-alignment and increased muscle tightness can lead the patient into a lifelong struggle with musculoskeletal pain.
Thus it can be easily understood that our posture is a major factor in our overall health and wellbeing. People with non-twisting feet usually have naturally good posture, less joint and muscle pain and fewer visceral problems than people with the PMS foot structure (which causes twisting feet) and the resulting kyphotic posture.
References
[1] Wheaton C. Mandibular Rest Position: Relation¬ship to Occlusion, Posture and Muscle Activity. In: New Concepts in Craniomandibular and Chronic Pain Management. London: Mosby-Wolf. pp. 163-75; 1994.
[2] Miliani R, et al. Relationship between Dental Occlusion and Posture. Journal of Craniomandibular Practice. pp. 127-133. Vol 18, No 2. 2000.
[3] MacConkey D. The relationship of posture and dental health. International Journal of Orofacial Myology. Vol 17. No 3:8-10; 1991.
[4] Irvin R E. Is normal posture a correctable Origin of common, chronic, and otherwise idiopathic dis¬comfort of the musculoskeletal system? In Vleeming A, Mooney V, Dorman T, Snijders C, Edits. Second Interdisciplinary World Congress on Low Back Pain, San Diego. pp. 425-460; 1995.
[5] Cathie A. The influence of the lower extremities upon the structural integrity of thebody. 1950. In: Postural Balance and Imbalance. Peterson B, ed. Indianapolis: American Academy Of Osteopathy. pp. 50-53; 1983.
[6] Fink M, Wahling K, Stiesch-Scholz M, et al. The functional relationship between the craniomandibular system, cervical spine and sacroiliac joint: a preliminary study. Cranio 21: 202-08; 2003.
[7] Donatelli R. The Biomechanics of the Foot and Ankle, 2nd Edit. Philadelphia: F A DavisCo. Pg. 55-59; 1996.
[8] Nicolakis P, Nicolakis M, Piehslinger E, Ebenbichler G, et al. Relationship between craniomandibular disorders and poor posture. Cranio April 18(2):106-12; 2000.
[9] Rothbart B A, 2002. Medial Column Foot Systems: An Innovative Tool for Improving Posture. Journal of Bodywork and Movement Therapies (6)1:37-46; 2002.
[10] Streeter G L. Developmental horizons in human embryos. In
Contributions to Embryology, Vols. 21, 32, 34. Washington DC. Carnegie Institution of Washington, 1945,1948,1951.
[11] O'Rahilly R, Gardner E. The timing and sequence of events in the development of the limbs in the human embryo. Anatomical Embryology, 1-23, 1975.
[12] Jirasek J E, Keith L G. An Atlas of the Human Embryo and Fetus: A photographic review of human prenatal development. CRS Press, Parthenon Publishers, 1st edition, 2001.
[13] Sewell R S. A study of the astragalus (talus). Part IV. Journal Anatomy
Physiology, Vol 40:152; 1906.
[14] Straus W L. Growth of the human foot and its evolutionary significance.
Contributions in Embryology 19:95; 1927.
[15] McPoil T, Cameron J A, Adrian M J. Anatomical characteristics of the talus in relation to forefoot deformities. Journal American Podiatric Medical Association 77(2): 1987.
[16] Sarrafian K S. Anatomy of the Foot and Ankle: Descriptive, Topographic, Functional. 2nd Ed., Lippincott Williams & Wilkins, Feb 1993.
[17] Tax H R. Podopediatrics. Baltimore: Williams & Wilkins, 1980.
[18] Hlavac H F. Compensated forefoot varus. Journal Podiatric Medical Association 60(6):229-233; 1970.
[19] Daniels T R, Smith J W, Ross T I. Varus Malalignment of the Talar Neck. Its Effect on the Position of the Foot and on Subtalar Motion. Journal Bone Joint Surgery; 78:1559 – 1567; 1996.
[20] Cummings G S, Higbie E J. A weight bearing method for determining forefoot posting for orthotic fabrication. Physio Research Intern, Vol 2(1):42-50; 1997.
[21] Rothbart B A. Relationship of Functional Leg-Length Discrepancy to Abnormal Pronation. Journal American Podiatric Medical Association 96(6):499-507; 2006.
[22] Kuchera M. Gravitational Stress, Musculoliga¬mentous Strain, And Postural Alignment. In: Spine: State of the Art Reviews. Philadelphia: Hanley & Belfus. Vol. 9, No 2, May 1995.
[23] Rothbart B A. Vertical Facial Dimensions Linked to Abnormal Foot Motion. Journal American Podiatric Medical Association, 98(3):01-08, May. 2008.
[24] Rothbart B A, Yerratt M. An Innovative Mechanical Approach to Treating Chronic Knee Pain: A BioImplosition Model. The Pain Practitioner (formerly American Journal of Pain Management) 4(3):13-18; 1994.
[25] Rothbart B A. Tactile therapy shirts patients toward equilibrium. Biomechanics. Vol XII, No 10:61-68; 2005.
[26] Winston D B, James P C, Stinear C M, Fleming M K, et. al. Functional Connectivity Between Secondary and Primary Motor Areas Underlying Hand-Foot Coordination. Journal Neurophysiology 98:414-422; 2007.
[27] Emmanuel G, Lehéricy S, Pochon J P, Tézenas du Montcel S, et.al. Foot, Hand, Face and Eye Representation in the Human Striatum. Cerebral Cortex, Vol.13(2):162-169; 2003.
[28] Paus R, Theoharides T C, Arck P C. Neuroimmunoendocrine circuitry of the ‘brain-skin connection’. Trends in Immunology, Vol.27(1):32-39; 2006.
[29] Davis J. Nervous System Connection - The Brilliant Link Between the Brain and Body. Ezine Article. Online: http://ezinearticles.com/?Nervous-System-Connection---The-Brilliant-Link-Between-the-Brain-and-the-Body&id=4242937
[30] Rothbart B A, Penzabene L F. Forever Free From Chronic Pain. 2nd Ed., Happy About Publishers, California. 2009.
[31] Nelson C. Postural analysis and its relation to systemic disease. In: Postural Balance and Imbalance. Peterson B, ed. Indianapolis: American Academy of Osteopathy, 16-19; 1983.
[32] Rothbart BA, Esterbrook L. Excessive Pronation: A Major Biomechanical Determinant in the Development of Chondromalacia and Pelvic Lists. Journal Manipulative Physiologic Therapeutics 11(5): 373-379. 1988.
Comments:
-
Professor/Dr Rothbart said..
Error Correction 1:
Directly under Figure 2, it should read:
Rothbart suggests that if talar torsion is GREATER than 35 degrees this results in a planter grade foot. That is when the subtalar joint is placed in its anatomical neutral position, the entire forefoot rests on the ground. (See Figure 2)
Error Correction 2:
Directly under Figure 3, it should read:
Rothbart also suggests that if the talar torsion is LESS than 35 degrees, when the subtalar joint is in its anatomical neutral position, the 1st metatarsal and hallux do not rest on the ground.