Positive Health Online
Your Country
Piriformis Syndrome
listed in osteopathy, originally published in issue 202 - January 2013
Outline
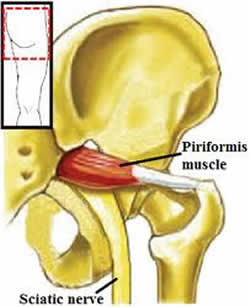
A referred posterior leg pain condition described as a compression or irritation of the sciatic nerve by a contracted or stretched piriformis muscle. The syndrome is six times more common in females than in males.
Cause
Overstrain to the sacroiliac joint produces a ligamentous sprain, leading to a reflex shortening of piriformis muscle, compression and irritation of the sciatic nerve sheath caused by biochemical agents released from an inflamed piriformis muscle, where the two structures meet at the greater sciatic foramen. In anatomical variations, the sciatic nerve penetrates piriformis (10% UK population). Prolonged sitting, buttock trauma, leg length discrepancy, and hip flexor tightness are among other causative factors.
Signs and Symptoms
Pain Pattern
Pain and paresthesia may travel the course of the sciatic nerve. Either deep boring or dull ache down the posterior thigh to the knee, occasionally extending to the foot, occurs.
Palpation
Digital palpation reveals trigger points and spasms at the site of the piriformis muscle. Gluteals may be tender, and tightness and stiffness of the hamstrings and low back might occur. Deep pressure over affected piriformis reproduces sciatic pain.
Range of Motion
Internal rotation of hip with knees flexed is painful.
Orthopaedic Tests
Positive straight leg raise with pain intensified by simultaneous internal rotation of the leg and relieved by external rotation (piriformis test).
Valsalva’s maneuver (-ve)
Straight leg raise (+/-)
Neurological Tests
Radiation pattern mimics sciatica, but with an absence of true neurological findings
Toe, heel walk (-ve)
Medipin (-ve)
Reflexes (-ve)
Motor (-ve)
Other Manifestations
Symptoms are almost identical to lumbar PID.
Differential Diagnosis
- Sciatica/ Referred pain;
- Compression of the posterior femoral cutaneous nerve;
- Sacro-iliac joint strain;
- Inominate Fracture;
- Gluteal / Hamstring tear / strain;
- Lumbar Prolapsed Intervertebral disc (PID).
Radiological Findings
Soft tissue injury, therefore Unremarkable
Clinical Note
Piriformis syndrome is often misdiagnosed as sciatic pain and numbness in the posterior thigh, which is more logically compression of the posterior femoral cutaneous nerve; true sciatic referral will pass down and into the foot. palpation of the piriformis muscle and by the presence of trigger point tenderness of the muscle adjacent to the sacrum.
Piriformis ‘Drop Test’: Patient prone, knees flexed at 90 degrees, the tibias are allowed to fall laterally, causing the hips to rotate internally. Operator stands at caudal end of table, comparing each side for the amount of internal rotation. Decreased rotation internally concurrent with other findings may indicate tight piriformis.
Treatment Aims
- Reduce hypertonia of piriformis;
- Relieve pain and prevent recurrence;
- Assess movement of the sacro-iliac joints and check for pelvic rotation.
.jpg)
Osteopathic Approach to Treatment
Acute phase
- Ice packs to promote vasoconstriction to decrease inflammation, pain, oedema, and muscle spasms. Ice packs over affected area for 20 minutes with dry towel between ice packs and subject. Ice, ultrasound (pulsed), and dry needling may be used. Interferential current for pain and oedema management.
Chronic phase
- Moist hot packs to affected area for 10 minutes to relax the muscle and increase blood flow, ultrasound-electrical muscle stimulation combination: acute (pulsed), chronic (continuous). Combination therapy facilitates healing, decreases pain and spasm;
- Muscle work, including trigger point therapy, myofascial release, spray and stretch techniques, and massage, to recondition muscles and prevent fibrotic adhesions. Screen piriformis musculature closely for spasms and tender points;
- Manipulation: Determine if there is joint locking of the sacro-iliac joint / pelvic rotation and manipulate. Manipulation helps improve sacro-iliac ROM and prevent fibrotic adhesion.
Clinical Note
On the evidence, particularly the most scientifically valid clinical studies, manipulation applied by Osteopaths is shown to be more effective than alternative treatments for piriformis syndrome. (Ref needed) Many medical therapies are of questionable validity or are clearly inadequate.
.jpg)
Inhibition and Muscle Energy Techniques (MET) to Piriformis
- Locate piriformis (external rotator of hip) get patient to ext rotate the hip against resistance palpate to locate;
- Using re-enforced thumbs or elbow as applicator, with the patient prone using a pillow under the abdomen to prevent hyperextension of the lumbar spine.
Remember; the patient may have facet capsular irritation/ spondylo-arthrosis of the L Spine. If the patient is elderly place in a side lying position.
- Be aware of sciatic.n and Lat.fem cutaneous nerve (S1, 2,3);
- Use applicator to apply direct inhibition for approx 15seconds, more if the patient is fit less if the patient is older or more sensitive. Repeat 4 or 5 times until you feel tissue change. Back off and re-position if you have compressed the sciatic nerve, move laterally!
- MET with patient’s knee flexed to 90˚, resist external rotation; metric place stretch at end; lytic you win. This technique is useful for not just piriformis but the deep external rotators (gamelli and obturators).
Patient Advice/Self Directed Exercise Programme
Instruct patient to:
- Get adequate rest on a firm mattress;
- Avoid heavy lifting or bending postures;
- Sleep supine with pillows under the knees or on the side with pillows between the legs;
- Perform piriformis stretch per instruction i.e.;
- Piriformis stretch: patient supine, lumbar spine flattened against the floor, bend knee to waist level, crosses the affected leg over the other leg. Patient then gently pulls the unaffected leg towards their chest, hold for 10 to 15 seconds. Fifteen repetitions twice a day.
Comments:
-
No Article Comments available